What is an ACJ stabilisation?
The ACJ is between your collar bone (clavicle) and the acromion (which is the top part of the shoulder blade on the outer edge of the shoulder). If this joint is injured, it may become displaced and unstable. Sometimes surgery is required to repair it. This involves repairing the torn tendons or replacing them with either natural or artificial ligaments (Figure1).
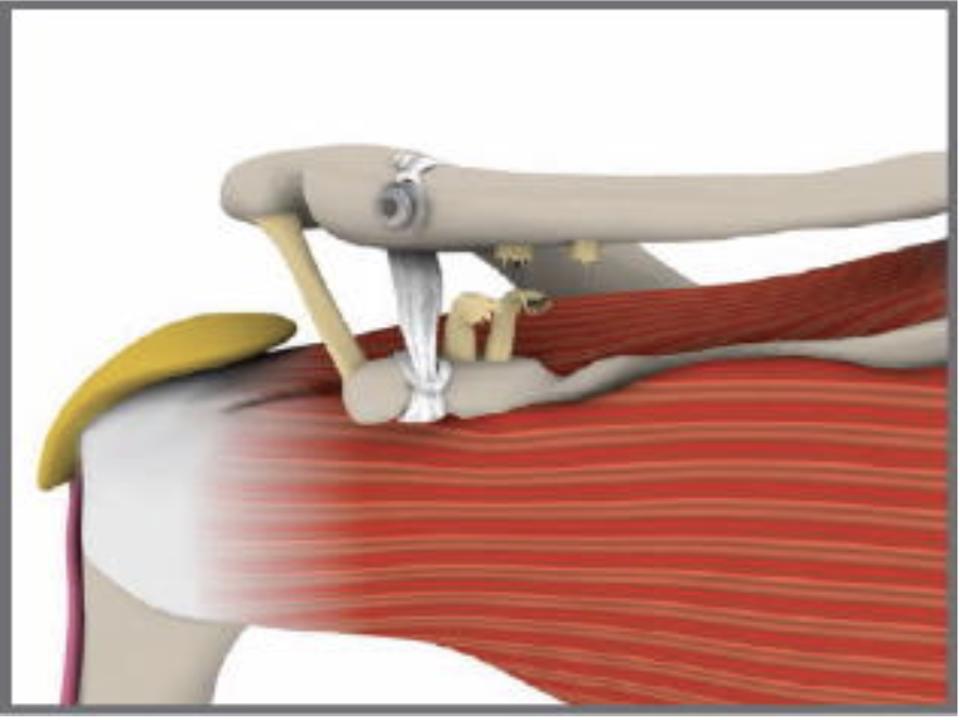
Figure 1: Example of a Nottingham Lockdown ACJ Repair
Why should I have an ACJ stabilisation?
The main reason for needing this surgery is pain resulting from the instability of the ACJ. By replacing the ligaments, your shoulder should feel less painful, and you should have improved function.
Exercises
You will perform only shoulder girdle, elbow, wrist, and hand exercises in the first 4 weeks. These are the exercises you need to do to prevent the arm becoming stiff when you are in the sling. The physiotherapist will go over the exercises with you before or after your operation.
- With your arm in the sling: move your hand up and down at the wrist. Repeat 5 times.
- With your arm in the sling: make a tight fist with your fingers then stretch the fingers straight. Repeat 5 times.
- With your arm in the sling: keep the elbow bent at your side, turn the hand to face the ceiling and then the ground. Repeat 5 times.
- With your arm in the sling: regularly pull your shoulder blades back and together, hold for 5 seconds, and then relax. Repeat 5 times.
- With the arm out of the sling: bend and straighten the elbow (do this when washing and dressing). Repeat 5 times.
Repeat exercises 1. to 4., four times daily. Do exercise 5. once daily.
Continue these exercises until otherwise advised by your physiotherapist.
If you require further information, please discuss this with the doctors, nurses, or physiotherapist either during your stay in hospital or in clinic.
Follow up appointments
An appointment will be sent to attend the Orthopaedic Outpatient clinic 5 weeks after your surgery. You will be seen by the consultant or registrar. You will have a check x-ray on arrival.
You will need to arrange an appointment at 14 days to have the wound checked by the practice nurse at your general practitioner (GP) surgery. The nursing staff will advise you.
You will be contacted, and a physiotherapy appointment will be arranged after you go home. You will start your outpatient physiotherapy 4 weeks after the operation. At this time the sling can be removed.
Advice after the operation
Pain
A nerve block may be used during the surgery. This means that immediately after the operation the shoulder and arm often feel completely numb. This may last for a few hours. After this the shoulder may well be painful, and you will be given painkillers to help ease this when in hospital. Please continue to take the painkillers as advised by the nursing staff or doctor after you are home.
Ice packs may also help reduce pain. Wrap crushed ice or frozen peas in a damp, cold cloth and place on the shoulder for up to 15 minutes. Do not apply ice packs when the shoulder and arm still feel numb.
Advice after the operation
You will return from theatre wearing a sling. The sling must be worn at all times for 4 weeks.
You will be expected to remove the sling for washing, changing your t-shirt or vest and elbow exercises only.
Your physiotherapist will advise and demonstrate these activities.
The shoulder must remain immobilised with the sling and the body belt for 4 weeks. You should only wear a loose vest or t-shirt under the sling. All other clothes: shirt/blouse or jumper/cardigan/coat should be worn over the sling.
Advice after the operation
There is an incision at the front of the shoulder. The stitches are dissolvable. Keep the wound dry until it is well healed.
The nursing staff will provide you with dressings to cover the wound until it is healed.
If your wound changes in appearance, weeps fluid or pus or you feel unwell with a high temperature, contact your GP.
Dressing
In the sling, you can wear one item of clothing under your sling i.e. baggy t-shirt or vest. When dressing:
- Lean forward slowly, allowing your arm to hang down.
- Feed the t-shirt or vest sleeve up the operation arm, then over your head.
- Then dress the good arm.
Do not twist or lift the operation arm when dressing.
When undressing always undress the good arm, then the head, then the operation arm last.
Washing
It is important to keep your skin in good condition. To take off the sling in sitting:
- Remove the velcro straps from your forearm and remove the sling.
- Support the forearm with your good hand and gently allow the elbow to straighten as you stand up.
- Lean forward slowly and allow your arm to hang down.
- Wash and dry thoroughly under your arm then reapply the sling.
- Try to do this daily.
Do not twist or lift the operation arm when washing.
Driving
You will not be able to drive for a minimum of 6 weeks. Your surgeon will confirm when you may begin driving again. You may be required to speak to your vehicle insurance provider before driving.
Return to work
This will depend on your injury, your progress after the operation and your occupation. You will need to discuss this with your consultant.
Return to leisure activities
This will depend on your injury and your progress after the operation. Your physiotherapist and surgeon will advise you when it is safe to get back your normal leisure activities.
Worries or concerns
For non-urgent issues/concerns
For non-urgent issues or concerns please contact your consultant’s secretary through the NHS Fife Hospital switchboard 01592 643355.
For urgent concerns
If you have any urgent concerns regarding your operation, please contact the service:
Urgent advice for patients with post-surgical problems between the hours of 8am to 4pm Monday to Friday please contact the National Treatment Centre-Fife Orthopaedics 01592 643355 Extension 22685.
Urgent advice for patients with post-surgical problems between the hours of 4pm to 8pm Monday to Friday, Saturday, Sunday and Public Holidays 8am to 8pm please contact National Treatment Centre-Fife Orthopaedics - advanced nurse practitioner 01592 643355 Extension 22685.
Urgent out of the above hours advice:
For an urgent problem out of hours please contact NHS 24 on 111 or attend the Accident & Emergency Department.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.




