Fife Musculoskeletal Physiotherapy
This information has been developed to supplement the information the Doctor or Healthcare Practitioner has already given you.
Issue No: 4.1.1.5.5.1
Date of Issue: February 2025
Review Date: February 2026
If the review date has passed, the content will apply until the next version is published.
Introduction
The purpose of the enclosed information is to:
- Help you understand more about Frozen Shoulder (sometimes called adhesive capsulitis).
- Guide you through a home rehabilitation programme (a series of exercises and other measures completed in your home, which are designed to ease your symptoms and speed your recovery).
What is a frozen shoulder?
Frozen shoulder is a condition that causes pain and stiffness of the shoulder joint. The shoulder joint is covered by a structure called the joint capsule. The capsule contains and produces the lubricating fluid for the joint. In the shoulder the capsule extends easily to allow the shoulder to move freely. In a frozen shoulder the capsule can become inflamed and tighten (Figure 1). This causes pain and stiffness of the shoulder.
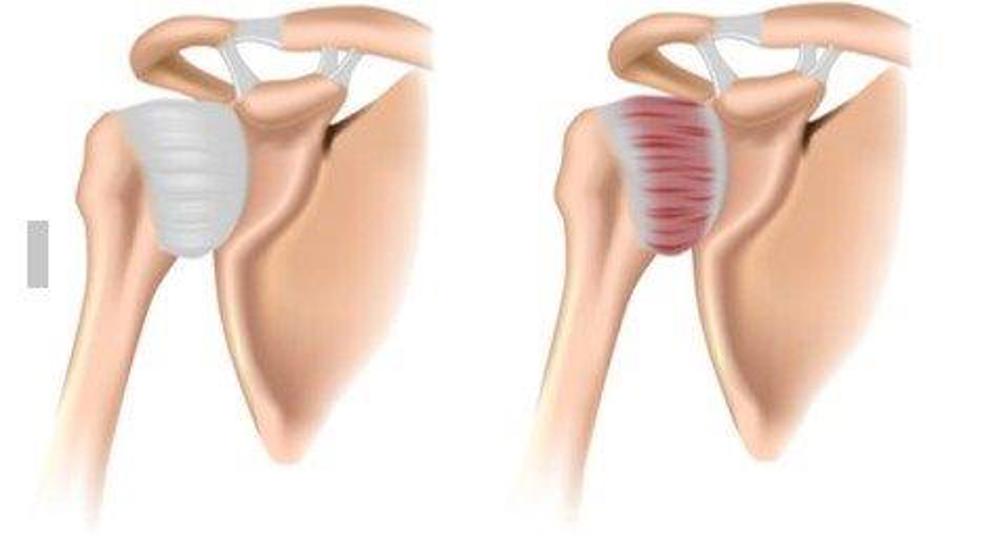
Figure 1: Shoulder affected by frozen shoulder
What are the symptoms?
Frozen shoulder symptoms tends to develop gradually and have two main phases. These are the pain dominant phase and stiffness dominant phase.
Pain dominant phase
In this phase pain can be typically felt in and around the shoulder joint. Sometimes pain can radiate into the upper arm and forearm. Pain can be worse at night while sleeping. Day to day activities can be quite painful, especially when trying to take the arm above shoulder height and also behind the back.
Stiffness dominant phase
In this phase the severity of pain tends to decrease. The main issue tends to be stiffness of the shoulder causing restricted movements of the arm in all directions. This can have an impact on your work, hobbies and activities of daily living.
What are the causes?
The exact cause of frozen shoulder is uncertain. Healthcare professionals categorise the condition as either Primary or Secondary depending on the probable causes. Frozen shoulder is more common in women, in individuals aged 40 to 65 years old, and in people who are diabetic.
Primary (or Idiopathic) frozen shoulder is when the exact cause is unknown. It is more common in people with a history of diabetes, high cholesterol, thyroid problems or Dupuytren’s contracture of the hand.
Secondary frozen shoulder can develop if the shoulder and the arm is kept still for a prolonged period. This can be following a stroke, heart attack or after surgery to the shoulder. It can also occur following injuries to the shoulder such as a fracture of the shoulder or an injury to the rotator cuff muscles.
How is it diagnosed?
Frozen shoulder is diagnosed through a clinical examination and by signs and the symptoms you report.
Should I have an x-ray or scans?
Sometimes an x-ray is requested to check if there are any bone or joint abnormalities in the shoulder joint.
What is the prognosis?
In most cases the condition will show complete or near complete recovery even without any treatment interventions. On average it can take 2 to 4 years for symptoms to fully resolve. If your symptoms are not improving, you may be referred to a physiotherapist for advice and physiotherapy treatment. In a few cases you may need referral to an Orthopaedic Surgeon for consideration of further interventions.
Is frozen shoulder serious?
Frozen shoulder can be very painful, but is fortunately not usually serious.
What are the treatment options?
First Line Treatments
- Self-management advice and exercises to improve mobility of the shoulder.
- Consult your GP or pharmacist to get advice on pain medication.
- Depending on your past medical history, your GP may prescribe Non-steroidal Anti-Inflammatory Drugs (NSAIDs).
Second Line Treatments
- Physiotherapy which may involve targeted exercises to reduce pain and improve strength and mobility of the arm.
- Your GP or healthcare professional may suggest a shoulder joint injection. This is a corticosteroid injection which may help to reduce pain and inflammation in your shoulder.
Third Line Treatments
The following options are usually only considered after first and extensive second line treatments have failed to improve symptoms. This is usually after approximately 3 to 6 months.
- Distension arthrogram is a procedure done under x-ray guidance where a mixture of fluid and air is injected into the shoulder joint capsule. This creates a stretching of the tissues which are causing stiffness of the shoulder.
- Manipulation Under Anaesthesia (MUA). This is an orthopaedic procedure where the shoulder joint and its tissues are stretched under a general anaesthetic.
- Arthroscopic or Open Capsular Release, if the above methods fail to improve the symptoms, a keyhole or an open surgery is performed to release the capsular tissue in the shoulder joint.
What can I do myself to help frozen shoulder symptoms?
The following actions may help you manage your pain.
Heat: you may want to apply a heat pad or a hot water bottle with an insulated cover on the shoulder and upper arm. Please make sure this is not too hot and the hot pack or bottle has a suitable cover. You should do this for 10 to 15 minutes, 3 to 4 times a day. A hot bath or shower can also help ease symptoms.
Ice: wrap crushed ice in a damp towel, hold it against the part of your shoulder or arm that is sore for 5 to 10 minutes. Make sure you use a damp towel between the ice and the skin to avoid ice burn. Alternatively, you could try sports sprays or gel packs. You can do this every 2 to 3 hours.
Home based rehabilitation programme
It is important that you have an active role in the management of your condition and that you work with your physiotherapist to maximise your recovery.
What you can do to help recovery will depend on the phase of frozen shoulder you are currently in. The following section will guide you through some basic advice and exercises which you can do in each of the phases described above.
How often should I do these exercises?
Stretching
There is no exact stretching time that works for everyone. Current evidence suggests stretching for 30 to 60 seconds in total may be optimal. This could be one or two sets of 30 second holds or three sets of 20 seconds.
It is, however, best to start with one or two stretches held for 10 or so seconds and gradually build this up to between 30 and 60 seconds. Stretching can feel uncomfortable, but should not feel painful during or after the exercise.
Rehabilitation exercises
Try to do these exercises once a day on most days. It is important to have rest days, especially if you are not used to exercising regularly. It is acceptable to break the exercises into groups and complete these at different times in the day.
Start with one set of 5 to 10 repetitions. As the exercise becomes easier you can either gradually increase the repetitions or add another set of exercises. A total of 45 repetitions would be a maximal effort i.e. 3 sets of 15 repetitions. Take a rest of up to a minute between each set. Ideally the muscle(s) you are exercising should begin to feel fatigued by the end of the exercise however you should not be straining. It is normal to have some discomfort during exercises as long as it’s acceptable to you.
As you increase the repetition of exercises you should try to have a rest day after each exercise day to allow your muscles to recover.

1. Pendulum
Let your affected arm hang relaxed straight down. Start with a small movement swinging your arm forwards and backwards.

2. Pendulum to the side
Stand leaning on a table with one hand.
Lean forward from the hips, relax the affected shoulder and gently swing the arm from side to side in front of you supporting with the other arm.

3. Pendulum circles
Stand leaning on a table with one hand.
Let your other arm hang relaxed straight down. Swing your arm as if drawing a circle on the floor. Change direction.
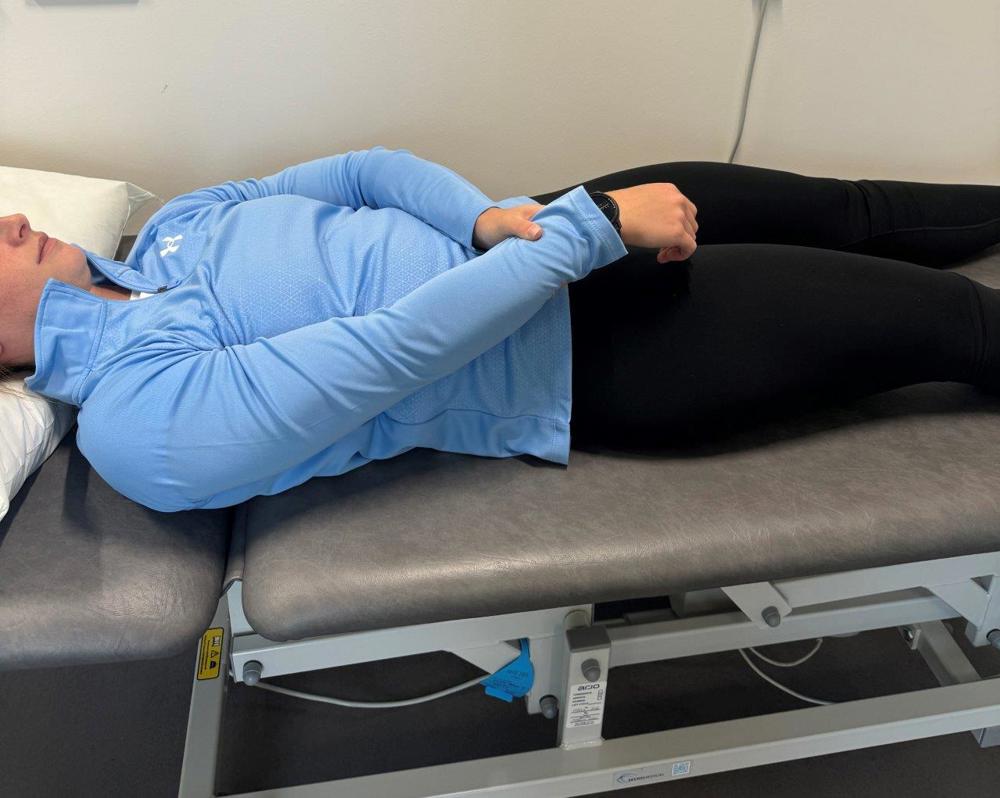

4. Supine assisted shoulder flexion (forward movement)
Lie on your back with your elbows bent.
Lift your injured arm with your other hand. Gradually increase the stretch depending on your pain. You should not push or force your arm during this exercise.
You may find it easier if you can hold a pole, walking stick or long umbrella in both hands to do the movement.

5. Shoulder pulley
Pull a rope through a ring located high above your head. Sit with your back against a wall. Hold onto both ends of the rope.
Lift your injured arm to 90 degrees, assist by pulling down with the other hand.
If your pain is manageable gently increase the height.
Phase 2: Stiff phase
If you can manage the early exercises described above, with minimal pain or discomfort you can progress to some more advanced exercises.
Aims:
- To increase range of movement without aggravating your pain.
- To reduce stiffness of the shoulder joint.
1. Shoulder flexion
Lying on your back with knees bent. Lift your arms straight up initially to shoulder height, if your pain is manageable, gradually increase the stretch. You should not push or force your arm during this exercise.
You may find it easier if you can hold a pole, walking stick or long umbrella in both hands to do the movement.

2. Table slide
Sit or stand. Place your hands on a table.
Slide your hand (injured side) along the table as far as you can without lifting your shoulders.

3. Butterfly stretch (s)
Sit or stand. Place your hands behind your neck, elbows pointing forward.
Move your elbows out to the side.

4. Internal rotation: Hand behind back
Stand with arms behind your back. Grasp the wrist of the arm you want to exercise.
Slide your hands up the back.

5a. Abduction arm to the side
Slide the ball to the side and let the ball roll under your hand.
Or if you do not have access to a ball try Exercise 5b instead:

5b. Abduction arm to the side
Lift your arm to the side, assisting the movement with your other hand.

6. Shoulder external rotation
Lie on your back with one elbow at a right angle.
Place a rolled towel under the elbow. Hold a stick with both hands.
Push the stick to move the arm outwards as much as your pain can tolerate. Hold for 10 to 20 seconds.
Repeat 3 to 5 times.
Phase 3: Recovery phase
If you are managing Phase 2 exercises without aggravating your symptoms, you should continue with the exercises until your symptoms have settled and range of movement has significantly improved. If you feel that you are progressing well, you may wish to begin a more active exercise regime such as swimming or light gymnasium work involving exercises, like the Phase 3 exercises outlined in this information.
Criteria for Progression onto Phase 3:
- If you are managing Phase 2 exercises without pain and discomfort.
- Minimal pain at the shoulder and upper arm
- No night pain and sleep disturbance
- If your pain at rest is below 4 out of 10 (pain scale: where 0 = no pain and 10 = worse pain imaginable).
- If you can put weight on your injured arm without pain and significant discomfort.
Aims:
- Improve dynamic strength of the upper limb
- Improve function
- To return to moderate intensity of exercises.

1. Wall pushes
Wall Push Up
Stand next to a wall. Place your hands on the wall, shoulder-width apart and fingers pointing upwards.
Keep the body in a straight line. Keep body in a straight line and shoulders down. Bend your arms and lower your chest towards the wall. Straighten your arms and push back away from the wall.

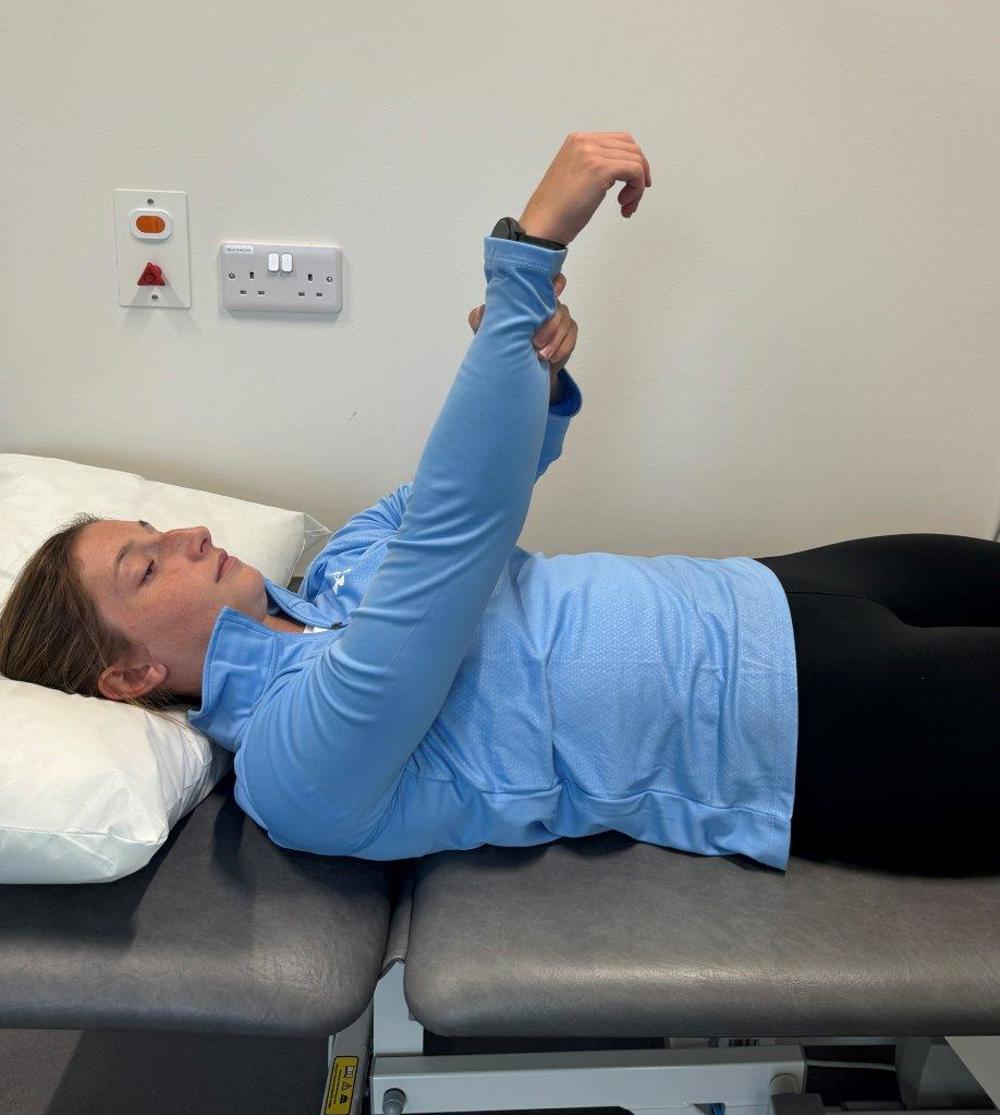
2. Weight lifts lying on back
Lying on your back, arm straight towards the ceiling holding a small hand weight or you can use a small grocery tin or small bottle filled with water.
Stretch your arm out further towards the ceiling.
Hold the weight up for approximately 6 to 10 seconds then slowly bring it down.

3. Shoulder pull backs
Stand leaning on a table with one hand.
Let your injured arm hang relaxed straight down.
Bend your elbow bringing it behind your back and pull your shoulder blades together.
If you wish to progress this exercise, hold onto a small dumbbell or weight (about 1 to 2 Kgs or whatever is an effort, but manageable).

4. Shoulder rotator cuff strengthening
Lying on the opposite side to your affected arm.
Holding a 1 to 2kg hand weight in your upper affected arm hand or you can use a small grocery tin or small bottle filled with water.
Keep your elbow at a right angle and support it against your side.
Lift weight towards the ceiling and lower back down.
Getting back to normal
Returning to activities of daily living
There are no specific time frames for returning to your usual activities and these vary from person to person. Symptoms may be ongoing for several months and you may need to adjust your activities and pace yourself during your recovery. Aim to increase your levels of activity gradually, avoiding worsening of your symptoms. Progress your activities as your symptoms and movements improve. It may take 18 months to 2 years to recover good functional movement of the shoulder.
Guidance for returning to work
Research suggests that staying active and keeping moving as pain allows, will help you get better sooner. Getting back to work helps most people with back pain. If you are ‘signed-off’ work, time frames for returning to work will depend on the type of work you do and a healthcare professional can advise on this. It is advised you communicate regularly with your employer to facilitate a safe and timely return to work.
Useful Information
NHS Inform
www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints
The Chartered Society of Physiotherapy
www.csp.org.uk/conditions/managing-your-bone-joint-or-muscle-pain
Worries or concerns
Should you have any worries or concerns, please contact your Physiotherapist or GP during working hours or contact NHS24 on 111 out of working hours.
If you continue to experience problems then you should consult a healthcare professional.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
