Fife Musculoskeletal Physiotherapy
This information has been developed to supplement the information the Doctor or Healthcare Practitioner has already given you.
Issue No: 4.1.2.15.1
Date of Issue: February 2025
Review Date: February 2026
If the review date has passed, the content will apply until the next version is published.
Introduction
This leaflet will provide you with information about greater trochanteric pain syndrome (GTPS) and how to manage your symptoms.
What is GTPS?
Greater trochanteric pain syndrome is a common and painful condition which affects the outside of the hip and thigh. It occurs when the tissues which lie over the outside of the hip (greater trochanter) become irritated. In many cases the pain is caused by overloading the soft tissues that attach to the outside of the hip (tendinopathy). In some cases a fluid filled pouch (bursa), which sits on the outside of the hip can also become inflamed.
What are the symptoms?
These vary from person to person. People may experience:
- Pain on the outside of the hip and thigh.
- Pain when lying on the affected side.
- Difficulty walking.
- Difficulty and pain going up and down stairs.
- Discomfort with certain activities.
What are the causes?
Often it can occur for no reason but there are various factors which appear to contribute to it. These are not fully known, but appear to be related to the hip structures not coping with heavy/frequent loads. GTPS is most commonly found in middle-aged women, however, it can affect anyone at any age. Other causes are:
- Direct trauma to the outside of the hip, such as a fall.
- Weakness in the gluteal muscles and tendons on the outside of the hip. If too much load is applied then this can cause the tissues to become inflamed.
- Prolonged running or walking.
- Excessive pressure to the outside of the hip e.g. being overweight.
How can I help manage my greater trochanteric pain?
Advice to help improve symptoms:
- Avoiding or decreasing the activities which cause your pain.
- Strengthening the muscles which support the hip.
- Spreading your weight evenly across both feet and not leaning on just one leg.
- Avoiding low chairs.
- Avoid sitting with your legs crossed.
- Losing weight if you are overweight.
- Using a handrail when going up or down stairs.
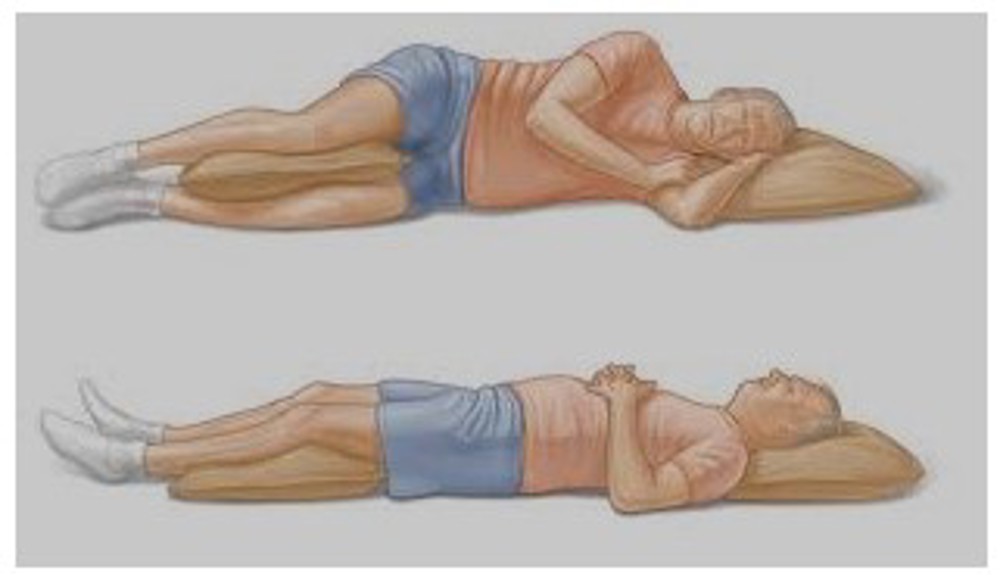
- Avoid sleeping on the painful side. Try lying on your back with a pillow under your knees or lie on your good side with a pillow between your legs to keep them in line with your hip joints.
- Try to keep active and stay at work even if you have to modify your duties.
- Apply an ice pack for 5 to 10 minutes two to three times a day. Make sure you place a damp towel between the ice and your skin to prevent an ice burn. Further information can be found on the NHS Inform website.
- Using painkillers to provide short term relief. Discuss these with your General Practitioner (GP) or pharmacist.
- If your pain is severe and you are unable to exercise, a corticosteroid injection may be useful in the short term to reduce your pain and enable you to function better. This should enable you to then exercise the injured leg to help resolve your condition. The injection will not resolve the cause of the problem and is not recommended as a first treatment option. This can be discussed with your GP or physiotherapist if there is a requirement for this.
How can physiotherapy help?
The best person to manage this condition is you! It is very important that you have an active role in the management of your condition and work with your physiotherapist to help improve your condition.
Your physiotherapist will carry out an assessment and help you decide on a treatment programme based on your individual needs. Advice and exercise from your physiotherapist are aimed to help you reduce your pain and manage your condition.
Early stage treatment
The initial goal of early treatment is to help settle your pain. It is important to reduce the pressure on the outside of your hip by avoiding or modifying activities which cause pain.
Pain relieving medications
As with any medication please speak to your GP, pharmacist or a suitably qualified healthcare professional for advice.
Exercises
Slowly building up the strength in the soft tissues on the outside of your hip is an important part of getting better. It is important that you know how much to exercise without making your pain worse and your physiotherapist can you advise on this. Try to avoid pain when exercising. Although it is acceptable to feel a little discomfort when exercising, this should not be excessive or last long. If in pain it is important you reduce the repetitions or intensity of the exercises so you minimise pain.
Your physiotherapist may also identify other specific treatments or exercises for you to complete. This will depend on your individual needs.


1. Bridging
Lie on your back with your knees bent and feet hip width apart.
Draw in your abdominals and tighten your buttocks. Tilt your pelvis backwards and slowly lift your pelvis up and then back one vertebra at time.
Lift only as high as you can while maintaining the pelvis position. Lower your pelvis down in a controlled manner.
Note: don’t let your lower back arch during the lift.
Repeat 10 times

2. Lying – static hip abduction
Lying on your back with legs straight and slightly wider than hip width apart.
Tie a belt or scarf around your lower thighs.
Very slowly and gently start to move your knees apart but only enough to take the slack up in the belt.
You should be aware of tension in the side of your hips/buttocks.
Hold 10 seconds and repeat 10 times.

3. Standing - static hip abduction
Stand tall, sideways close to a wall with affected leg bent at the knee and supported against the wall.
Press the knee against the wall and hold for 10 seconds.
Don’t let the knee of the leg you are standing on rotate inwards.
Repeat 10 times.

4. Mini squat
Stand tall with your feet approximately hip width apart and weight distributed evenly on both feet.
Bend your knees and hips as if you were sitting down.
Knees and toes should be pointing in the same direction.
Keep your knees over your toes as you squat.
Push back to the starting position using your front thighs and buttock muscles.
Repeat 10 times


5. Side stepping
Stand with your legs hip width apart and place an elastic band around your knees.
Step one foot out to the side, wider than hip width to the right and then repeat with the left.
The focus should be on a controlled push from one side and landing softly with control on the other.
The trunk should remain upright and the kneecaps should face straight ahead.
When stepping inwards, only step back to hip width. Do NOT bring your ankles together. Keep tension on the band at all times.
Repeat x 10 on both sides.
Later stage
The key to success is slow progressive loading of the soft tissues which are painful. If you continue to overload or underload the tendon it will remain painful and may lead to long standing problems.
Over time it is important to gradually increase the exercises to help the tendons and muscles become stronger and less painful and more able to cope with normal day to day tasks. Your physiotherapist will guide you with this if appropriate.
As with any exercise it is normal to feel discomfort or aching in your muscles 1 to 2 days after exercising. Often people will have a flare up of pain at some point. It is important to modify your exercises by reducing the repetitions or sets of exercise. Stop altogether if your pain is severe and discuss with your physiotherapist at your next appointment.
Prognosis
This condition often takes 6 to 12 months of rehabilitation to get settle, but this will depend on the cause.
It is normal to have flare ups during this time. If this happens, then it may be best to reduce the repetitions or rest for a few days before starting again.
In some cases a corticosteroid injection may be required to help alleviate pain. An injection, however, usually only provides temporary relief.
Useful Information
NHS Inform
www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints
The Chartered Society of Physiotherapy
www.csp.org.uk/conditions/managing-your-bone-joint-or-muscle-pain
Worries or concerns
Should you have any worries or concerns, please contact your GP during working hours or contact NHS24 on 111 out of working hours.
If you continue to experience problems then you should consult a healthcare professional.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
