Introduction
The purpose of this leaflet is to provide you information about hip osteoarthritis and how to best manage it.
What is osteoarthritis (OA)?
Osteoarthritis (OA) is the most common form of arthritis, and the hip is the second most commonly affected joint.
Everyone’s joints go through a normal cycle of wear and repair during their lifetime. As your joints repair themselves their shape and structure can change. If this happens in one or more of your joints, it’s known as osteoarthritis.
A joint is a part of the body where two or more bones meet. Your hip joint consists of a ball at the top of the thigh bone, which fits into a socket in your pelvis.
The ends of both bones in a joint are covered by a smooth slippery surface, known as cartilage. This is the soft, but tough tissue that allows the bones to move against each other without friction.
Osteoarthritis causes the cartilage in your hip joint to become thinner and the surfaces of the joint to become rougher. This can cause swelling, pain and stiffness, but not everyone will have these symptoms.
The exact cause of osteoarthritis is often not known, as there can be quite a few reasons why a person develops the condition. These include the genes inherited from your parents.
Osteoarthritis is sometimes called ‘degenerative joint disease’ or ‘wear and tear’ (Figure 1).
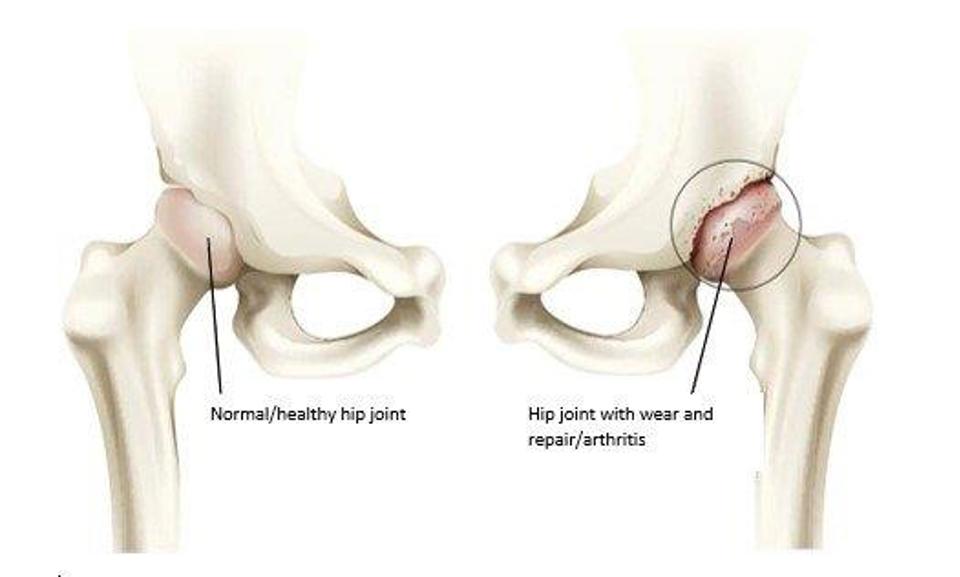
Figure 1 Front view of hip joint. A normal/health hip joint and hip joint with wear and repair/arthritis
What happens in osteoarthritis (OA)?
Normal joints are constantly undergoing repair because of normal wear. In some people, however, it seems that this repair process becomes faulty and osteoarthritis develops. A certain amount of wear and repair is normal as we age.
The pain is commonly felt in the groin area of front of the thigh. Any pain in your buttock, side of your thigh or below the knee is unlikely to be coming from the hip joint itself. Osteoarthritis of the hip does not cause altered sensation, pins and needles or muscle cramps.
What causes osteoarthritis (OA)?
Some of the many factors that may play a role in the development of osteoarthritis include:
- Age: Osteoarthritis becomes more common with increasing age. By the age of 65 at least half of the people will have osteoarthritis in some joint(s).
- Autoimmune Disease: Conditions such as rheumatoid arthritis can predispose to osteoarthritis.
- Increased Body Mass: Hip osteoarthritis is more likely if you are overweight, as increased load on the joints increases wear.
- Your Sex: Women are more likely to develop osteoarthritis than men.
- Genetics: Osteoarthritis is more likely if there is a history of joint problems in your family.
- Previous Joint Damage or Deformity: This may be from previous injury around the hip joint that has caused long term damage to the joint surfaces. There are some childhood hip conditions that can lead to osteoarthritis in the future.
In many cases unfortunately we do not know the exact cause of osteoarthritis.
What are the symptoms of hip osteoarthritis?
- Pain, stiffness and difficulty with movements of the joint are typical. The stiffness tends to be worse first thing in the morning, but can ease after an hour or so.
- Pain, stiffness and weakness around the hips can lead to problems walking, putting on shoes and socks and activities e.g. getting in or out of the car. Eventually it can disturb your sleep.
- A locking or cracking sensation around your hip can be common.
You may experience all or some of these symptoms. Your symptoms may vary for no apparent reason with bad spells lasting a few weeks or months broken by better periods.
How is hip osteoarthritis diagnosed?
Osteoarthritis is usually diagnosed based on your symptoms and also the physical signs found when your hip is examined. X-rays are usually used to confirm the diagnosis.
What can you do to help yourself?
There is no current cure for arthritis. There are, however, are number of options to manage your symptoms. These measures should allow you to maintain an active lifestyle.
Being active or exercise programmes
It is good to be active and exercise can help with symptoms. Focus on what you enjoy. Group exercise can help. Exercise is safe, but you should start gradually. It is normal to feel achy and tired at first. If pain keeps you awake at night and this lasts for a few days, then you may have done too much. If this happens, rest for a couple of days and as you feel better, gradually start again. If you don’t feel better discuss this with your health care professional.
There is no ideal exercise programme that suits everyone. Evidence suggests however that a mix of 1) aerobic exercise as such as walking, cycling or exercises in a swimming pool combined with 2) strengthening exercises for the muscles around the hip and 3) gentle hip movements/gentle stretching around the hip provide the best benefits. Activities that avoid impact joint loading such as cycling can be helpful. Swimming and aqua-aerobics can be particularly beneficial because the water supports your body’s weight so that less force goes through your joints as you exercise causing less pain.
It is important to find the right balance between rest and exercise. Exercise in moderation can help to reduce pain, maintain function and possibly delay the need for a hip replacement. The exercises at the back of this leaflet may be helpful (Appendix I).
Being a healthy weight
Being a healthy weight has been shown to significantly improve the symptoms of osteoarthritis. Pain, however, can make exercise and weight loss difficult. Some people find support groups can be helpful while trying to more active or be a healthy weight.
Walking aids
Some people find walking aids useful e.g. a walking stick(s) or walking poles. Walking aids can help take the weight off the hip which can help with pain, especially if you are walking longer than normal or on rough uneven ground. They make you more stable and less likely to fall. They also show people around you that you might need more space or are slower.
Reduce stress on the joint
Try not to overstress your joint by doing too much all in the one day e.g. spread household chores throughout the week. Avoid being in one position for too long when possible to help prevent stiffness.
Other options
Some people find purchasing a Transcutaneous Electrical Nerve Stimulator (TENS) machine, insoles or cushioned footwear are helpful. The evidence for these, however, is somewhat limited. Similarly, some people find supplements such as glucosamine or chondroitin are helpful, especially in the early stages. Again, there is limited evidence for these. There is, however, no evidence that these other options are harmful, provided you have no other medical conditions. It is best to ask your healthcare professional or pharmacist before using any of these.
Medication
If you still have pain after trying the above you can speak to your doctor who may discuss medication for pain relief. There are several different types of pain relief that your doctor can prescribe before thinking about having a hip replacement.
Surgery
Surgery for hip osteoarthritis is usually with a total hip replacement. Your healthcare team should always try other non-operative measures detailed above before suggesting a hip replacement. Surgery is usually only performed in patients with moderately severe or severe arthritis on their x-rays.
Not everyone with osteoarthritis of the hip will feel their symptoms are severe enough to consider a hip replacement. If your symptoms are still manageable and your medication is effective then you may prefer to wait. If you do not want surgery for your hip osteoarthritis at this time then you do not need to come to hospital to see an orthopaedic surgeon.
If your hip has significant osteoarthritis and your day to day quality of life is significantly affected by pain, stiffness and disability, and despite trying all the advice in this leaflet, a hip replacement may be considered.
Please note that 5% to 10% of patients who have hip replacement surgery are not satisfied with their hip replacement and a small number can develop serious complications as a result of the surgery.
Are there any reason why I cannot have a hip replacement?
Unfortunately, some people may not be able to have a hip replacement even though their osteoarthritis is very bad.
This may be because:
- You have a serious medical condition.
- You are at risk of falling.
- You have deep or long-lasting open sores (ulcers) in the skin of your leg, increasing your risk of infection.
- You have other medical conditions that put you at higher risk from an anaesthetic.
- It is important you are the best shape you can be prior to undergoing what is major surgery to ensure surgery is as safe as possible. If your weight and body mass index (BMI) is too high (BMI greater than 40kgs/m2) or too low (BMI less than 20kgs/m2) this may need to be addressed prior to surgery.
- If you are anaemic (too little iron in the blood) this may need to be corrected prior to surgery.
- If you are diabetic and your diabetic control is poor this again may need to be corrected.
Decisions about the timing of surgery will also consider the severity of the underlying hip arthritis.
What is a hip replacement and what risks are associated with it?
Hip replacement surgery is performed in ultra-clean theatres by a highly trained team of surgeons-anaesthetists-nurses. It is generally a very successful operation resulting in good pain relief and improved mobility. During the surgery the hip is replaced with an artificial joint (Figure 1).
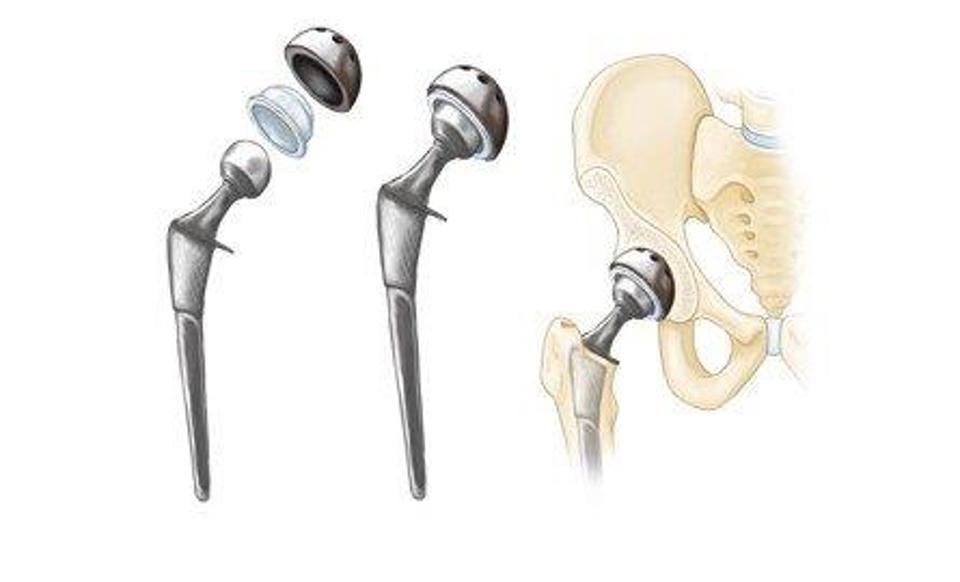
Figure 1: Diagram of a total hip replacement
What does a hip replacement procedure involve?
A hip replacement is a surgical procedure, in which the injured or damaged weight-bearing surfaces of the hip are replaced with artificial parts which are secured to the bone.
You will see the surgeon before your operation. They will take this opportunity to draw (mark with a pen) on your leg. This is to make sure they operate on the correct leg. You will also meet your anaesthetist who will discuss the type of anaesthetic with you. If you have any further questions that have arisen since your initial consultation this is a good time to ask.
You will receive a type of anaesthetic in the theatre prior to your surgery commencing. This may be a general anaesthetic (where you will be asleep) or a local block (e.g. where you are awake, but the area to be operated is completely numbed). The anaesthetist will discuss this with you.
We will clean your skin with antiseptic solution and cover the area with clean towels (drapes). The surgeon will make an incision (a cut) down the outside of the hip. Some of the muscles and tendons have to be cut away from the bone to gain access to the hip joint itself. Once this is done the worn out joint can be removed and an artificial joint one put back in. The joint will consist of a cup that sits in the pelvic bone, a stem the sits it the thigh bone and a head that sits on top of the stem.
When the surgeon is happy with the position and movements of the hip, they will close the tissue and skin. They may use stitches (sutures) or metal clips (skin staples). The clips and stitches will need to be removed around 10 to 14 days after the operation.
When you wake up, you will have a dressing on the outside of the hip. If you are in pain, please ask for pain killers. If you have pain, it is important that you tell the ward staff.
You new hip will be checked with an x-ray after your operation (sometimes on the same day) and we will encourage you to stand and walk either on the day of surgery or the latest by midday the day after the operation. Sometimes your x-ray will be performed when you come back for your post-operative check in the outpatient department.
You will be in hospital for as long as it takes for your pain to be under control and for you to be safe walking with crutches. It is important to note there will be pain and discomfort after surgery of this nature and this is quite normal. Some patients will go home the same day as their surgery and the vast majority (70%) by the following day.
The physiotherapy team will visit you, and suggest exercises for you. It is important to do these (as pain allows).
Please be aware that the surgeon who carries out your operation may either be your consultant or another surgeon who is well trained and/or supervised to perform your hip replacement.
Are there any risks with hip replacement surgery?
As with all surgical procedures, hip replacement carries some risks and complications.
Pain: Your hip will usually be sore for a few days/weeks after the operation. If you are in pain it is important to tell ward staff so they can give you pain relief medication. Pain will improve with time. Rarely, pain will be a chronic or long-term problem and may be due to any of the other complications listed below or for no obvious reason.
Dissatisfaction: The majority of patients are satisfied following hip replacement surgery, however, up to 10% of patients may experience some on-going discomfort in their hip and may not be entirely satisfied with their hip replacement. Up to 5% of patients may feel that they are worse off.
Other Common risks: (2% to 5%)
- Bleeding: Some patients may occasionally need a blood transfusion or iron tablets. Rarely, the bleeding may form a blood clot or large bruise within the hip which may become painful and may require an operation to remove it.
- Deep Vein Thrombosis (DVT): is a blood clot in a vein. The risks of developing a DVT are greater after any operation (and especially a bone operation). A DVT can pass in the blood stream and be deposited in the lungs a pulmonary embolism (PE). This is a very serious condition which affects your breathing. Your surgeon may give you medication to try and limit the risk of DVTs from forming. Some hospitals will also ask you to wear stockings on your legs, while others may use foot pumps to keep blood circulating around the leg. Starting to walk and moving about as soon as possible after your operation is one of the best ways to prevent blood clots from forming.
- The risks of DVT are increased in certain types of patients such as those with a family history of clots, those with other serious diseases such a kidney or liver disease and obesity. The biggest risk factors that you can do something about are obesity and smoking and you should try and address these before you even consider a hip joint replacement if you are overweight or smoke. This will significantly reduce your risk of clots.
- Altered leg length: the leg which has been operated upon may appear shorter or longer than the other. This can affect up to 20% of patients. It is occasionally managed with a heel raise on/in a shoe if it causes problems.
- Implant wear: With modern operating techniques and new implants, hip replacements last many years. In some cases, however, they may fail earlier. The reason is often unknown. The plastic bearing is the most commonly worn out part. If the replacement wears out or loosens it will become painful again and more surgery may be required. With newer designs of replacements, however, wear is becoming less of a problem than it was in the past.
- Overall around 90 to 95% of hip replacements will last 10 years.
Less Common: (1% to 2%)
Infection: We will give you antibiotics at the time of the operation and the procedure will also be performed in sterile conditions (theatre) with sterile equipment. Despite this infections still occur (up to 1% to 2%). The wound site may become red, hot and painful. There may also be a discharge of fluid or pus. We usually treat this with antibiotics and an operation to washout the joint may be necessary. In rare cases, the prosthesis may be removed and replaced at a later date. The infection can sometimes lead to sepsis (blood infection) and strong antibiotics are required in addition to further surgery.
Illnesses or medication that weakens the immune system such as diabetes, rheumatoid arthritis or immunosuppressant drugs increase the risk of infection as does obesity.
The biggest risk factors that you can do something about are obesity and smoking and you should try and address these before you even consider a hip joint replacement if you are overweight or smoke. This will significantly reduce your risk of infection.
If you are diabetic then having good control of your sugar levels (HbA1c levels <7% or <53mmol/mol) will again significantly reduce your risks of developing an infection following surgery.
Joint dislocation: If this occurs, the joint can usually be put back into place without an operation. Sometimes this is not possible, and an operation is required, followed by application of a hip brace. If your hip replacement remains unstable, further revision surgery may be required. The majority of dislocations occur in the first 12 weeks after surgery when the soft tissues are still healing so it is important you follow instructions from the nurses and physiotherapists.
Rare: (less than 1%)
- Pulmonary Embolism (PE): Is the spread of a blood clot to the lungs and can affect your breathing. This can be fatal.
- Altered wound healing: The wound may become red, thickened and painful (keloid scar) especially in Afro-Caribbeans. Up to 40% of patients have difficulty lying on their hip after surgery.
- Nerve Damage: Efforts are made to prevent this; however there is a risk of damage to the small nerves of the hip. This may cause temporary or permanent altered sensation around the outside of the hip. There may also be damage to the Sciatic Nerve and this may cause temporary or permanent weakness or altered sensation of the lower leg. Occasionally this may require the use of an ankle brace.
- Bone Damage: Bone may be broken when the prosthesis (false joint) is inserted. This may require fixing either during the operation or at a later date.
- Death: This very rare complication may occur after any major operation and from any of the above. Overall, the risk of dying after a hip replacement is very low, but death does occur in around 1:300 patients. The risk will be increased if you have medical problems such as heart or breathing problems and also increase with age. The risk of dying for someone aged over 80 for instance is over 1% and for those aged over 85 up to 3%.
We do not routinely provide a hospital appointment for osteoarthritis of the hip.
Further Useful Information
|
Versus Arthritis: |
https://versusarthritis.org/about-arthritis/conditions/osteoarthritis-oa-of-the-hip/
|
|
Hip and Knee Replacement General Advice: |
www.youtube.com/watch?v=xAL_TrQdtTY
|
|
General Persistent Pain Advice: |
https://youtu.be/C_3phB93rvI?si=rO7a24gN1HtKoVBd
|
|
Fife Sport and Leisure: |
This leaflet has been reviewed by patients and staff of NHS Fife.
Appendix 1
Useful Exercises:
Mobility/Stretching Exercises
Try to do these exercises every day, as stretching exercises can be particularly good for hip osteoarthritis. For these, it’s good to push until you start to feel the pain, but do not push through the pain, as it could make your symptoms worse.

1. Heel slide (stretch)
Lie on your back. Bend your leg and slide your knee towards you as far as is comfortable. Slide your heel down again slowly. Repeat 10 to 20 times. If this is comfortable or easy move to the exercises 2) and 3) below.

2. Knee lift (stretch)
Lie on your back. Pull each knee to your chest in turn, keeping the other leg straight. Take the movement up to the point you feel a stretch, hold for around 10 seconds and relax. Repeat 5 to 10 times. If this is difficult, try sliding your heel along the floor towards your bottom to begin with, and when this feels comfortable, try lifting your knee.

3. External hip rotation (stretch)
Lie on your back with your knees bent and feet flat, hip-width apart. Let one knee drop towards the floor and then bring it back up. Keep your back flat on the floor throughout.
Strengthening Exercises
To try and build up the strength of your muscles, try to do these exercises two to three times a week. You do not need to do them all, but choose ones you feel comfortably work the muscle around your hip.


4. Hip flexion (strengthening)
Position yourself near to a chair that you can use for support. Stand on one leg and bring the other one up to a right angle, then hold for up to 10 to 30 seconds. If you feel safe, challenge your balance by taking your hand off the chair. Instead of using your arm for support, you can also do this exercise by leaning against a wall and sliding your leg upwards along it.

5. Hip extension (strengthening)
Move your leg backwards, keeping your knee straight. Clench your buttock tightly and hold for five seconds. Do not lean forwards. Hold onto a chair or work surface for support.

6. Hip abduction (strengthening)
Lift your leg sideways, being careful not to rotate the leg outwards. Hold for five seconds and bring it back slowly, keeping your body straight throughout. Hold onto a chair or work surface for support. You can also do this exercise lying sideways.


7. Mini squat (strengthening)
Squat down until your kneecap covers your big toe, this should be at about 45 degrees. Hold this position for a count of five, if you can. Use a work surface or a chair for support if you need to.

8. Sit to stand (strengthening)
Sit on a chair and cross your arms, so that you don’t use them for support. Then repeatedly sit and stand, making sure your movements are slow and controlled. Repeat five times. You can make this exercise easier or more difficult by changing the height of the chair. You could do this by adding a cushion to the seat.

9. Heel to buttock exercise (strengthening)
Bend your knee to pull your heel up towards your bottom. Keep your knees in line and your kneecap pointing towards the floor.


10. Straight-leg raise (sitting)
Sit back in your chair, with your back straight. Straighten and raise one of your legs. Hold for a slow count to 10, then slowly lower your leg. Repeat 10 times with each leg.

11. Stomach exercise (strengthening/stabilising)
Lie on your back with knees bent.
Draw in your lower abdominal and pelvic floor muscles. Tilt the pelvis backwards so that your lower back flattens into the floor and hold for 10 to 20 seconds.

12. Leg raise (strengthening)
Lie face down. Tighten your stomach and buttocks muscles to lift one leg slightly off the floor, while keeping your hips flat on the ground. Hold this position for 5 to 10 seconds and repeat 3 times.

13. Quadriceps exercise (strengthening)
Pull your toes and ankles towards you, while keeping your leg straight and pushing your knee firmly against the floor. You should feel the tightness in the front of your leg. Hold for five seconds and relax. This exercise can be done from a sitting position as well, if you find this more comfortable.

14. Short arc quadriceps exercise (strengthening)
Roll up a towel and place it under your knee. Keep the back of your thigh on the towel and straighten your knee to raise your foot off the floor. Hold for 10 seconds, then lower slowly. Your physiotherapist might suggest holding this position for longer, sometimes for up to 30 seconds.
Diagrams reproduced courtesy of ©Physiotools
Aerobic Exercises
These exercises are best combined with aerobic exercises i.e. exercises that work the heart and lungs such as walking or cycling (or exercises in a swimming pool, if able).
If your symptoms do not improve within 6 weeks of doing these exercises you may want to seek advice from a physiotherapist.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
