Introduction
The purpose of this leaflet is to provide you information about knee osteoarthritis and how to best manage it.
What is Osteoarthritis?
Osteoarthritis is a condition that affects the joints causing pain and stiffness. The knee is one of the more commonly affected joints. It is sometimes referred to as degenerative joint disease or wear and tear.
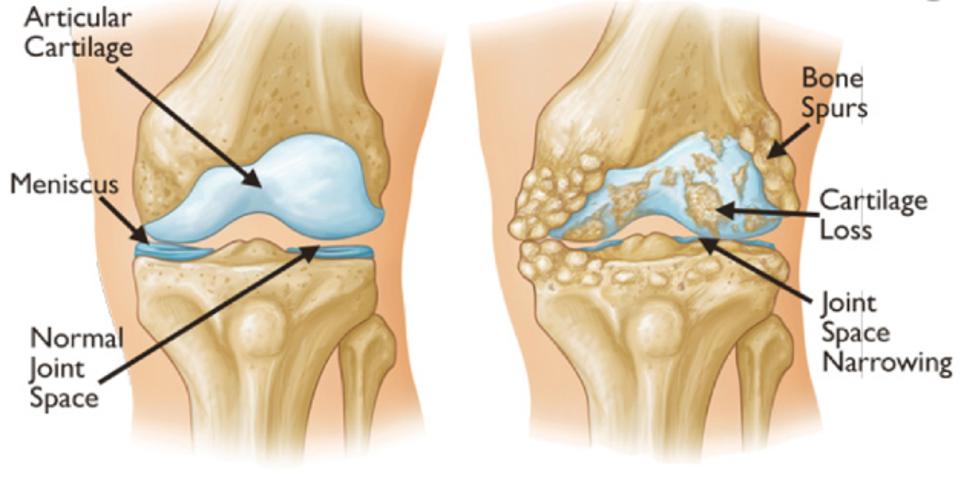
Figure 1: The drawing on the left hand shows the typical appearance of a healthy knee joint, and the right hand side is an arthritic knee joint
What causes Osteoarthritis (OA)?
All normal joints and joint tissues are constantly undergoing some form of repair because of the wear and tear that our daily activities place on them. In some people, however, it seems that this repair process becomes faulty (perhaps because of severe wear and tear to the joints or a problem with the repair process) and osteoarthritis develops. A certain amount of wear and repair is normal as we age.
In joints with osteoarthritis, the joint cartilage (otherwise known as Articular Cartilage) becomes damaged. The bone tissue next to the cartilage can also be affected and bony spurs can develop around the joint edges. Those spurs are called osteophytes and can sometimes been seen on X-rays. The joints and the surrounding tissues can also become inflamed. This inflammation is called synovitis.
Some of the many factors that may play a role in the development of osteoarthritis include:
-
Age
Osteoarthritis becomes more common with increasing age. By the age of 65 at least half of the people will have osteoarthritis in some joint(s). -
Autoimmune Disease
Conditions such as rheumatoid arthritis can predispose to osteoarthritis. -
Increased Body Mass
Knee osteoarthritis is more likely if you are overweight, as increased load on the joints increases wear. -
Your Sex
Women are more likely to develop osteoarthritis than men. -
Genetics
Osteoarthritis is more likely if there is a history of joint problems in your family. -
Previous Joint Damage or Deformity
This may be from previous injury around the knee joint that has caused long term damage to the joint surfaces.
In the majority of people, however, the exact cause of osteoarthritis is unknown. It is probably a combination of the above factors.
What are the symptoms of osteoarthritis (OA)?
Pain, stiffness, and limitation in full movement of the joint are typical. The stiffness tends to be worse first thing in the morning but tends to ease after half an hour or so. The pain tends to be worse while you are using the joint, however sometimes the pain can wake you at night even when the joint is being rested.
- Swelling and inflammation of the knee can sometimes occur.
- An affected joint tends to look a little larger or more knobbly than usual.
- A grating or cracking sound or sensation at your knee is fairly common.
- Weakness and muscle wasting around the knee joint can make it difficult to fully straighten the knee.
- Reduced function, such as problems with climbing stairs, walking for long distances, and kneeling.
You may experience all or some of those symptoms. Your symptoms may vary for no apparent reason with bad spells of a few weeks or months broken by better periods.
How is osteoarthritis (OA) diagnosed?
Osteoarthritis is usually diagnosed based on your symptoms and the physical signs that are found when your knee was examined. There are no blood tests for osteoarthritis. X-rays are often not needed to diagnose osteoarthritis. Sometimes, however, your doctor may suggest X-rays or other tests if they are uncertain about the diagnosis and want to rule out other problems.
What can you do to help yourself?
There is no current cure for arthritis. There are, however, are number of options to manage your symptoms. These measures should allow you to maintain an active lifestyle.
Being active or exercise programmes?
It is good to be active and exercise can help with symptoms. Focus on what you enjoy. Group exercise can help. Exercise is safe, but you should start gradually. It is normal to feel achy and tired at first. If pain keeps you awake at night and this lasts for a few days, then you may have done too much. If this happens, rest for a couple of days and as you feel better, gradually start again. If you don’t feel better discuss this with your health care professional.
There is no ideal exercise programme that suits everyone. Evidence suggests however that a mix of 1) aerobic exercise as such as walking, cycling or exercises in a swimming pool combined with 2) strengthening exercises for the muscles around the knee and 3) gentle knee movements/gentle stretching around the knee provide the best benefits. Activities that avoid impact joint loading such as cycling can be helpful. Swimming and aqua-aerobics can be particularly beneficial because the water supports your body’s weight so that less force goes through your joints as you exercise causing less pain.
Osteoarthritis in the knee can particularly weaken the thigh muscles (quadriceps). This can increase your knee pain and you may feel as if your knee has a tendency to give way perhaps even causing you to stumble or fall.
Generally, exercises that allow you to work on your thigh muscles while not putting too much stress through your knee joint are the best type. These are termed “Low Impact Exercises”. Types of Low Impact Exercises recommended include Cycling, Swimming, and Walking. High Impact Exercises, such as running or jumping, should be avoided. A physiotherapist in your local hospital or health centre can give you more advice on exercise and managing with osteoarthritis.
Leisure centres also run a variety of exercise classes that may be suitable and enjoyable. These classes can help to introduce you to exercise especially if you have not done it for quite some time.
It is important to find the right balance between rest and exercise. Exercise in moderation can help to reduce pain, maintain function and possibly delay the need for a knee replacement. The exercises at the back of this leaflet may be helpful (Appendix I).
Being a healthy weight
Being a healthy weight has been shown to significantly improve the symptoms of osteoarthritis. Pain, however, can make exercise and weight loss difficult. Some people find support groups can be helpful while trying to more active or be a healthy weight.
Walking aids
Some people find walking aids useful e.g. a walking stick(s) or walking poles. Walking aids can help take the weight off the knee which can help with pain, especially if you are walking longer than normal or on rough uneven ground. If using a walking stick ensure this is used in the other hand to where the pain is e.g. if you have pain in the left knee your stick should be used in the right hand. They make you more stable and less likely to fall. They also show people around you that you might need more space or are slower.
Reduce stress on the joint
Try not to overstress your joint by doing too much all in the one day e.g. spread household chores throughout the week. Avoid being in one position for too long when possible to help prevent stiffness .e.g. keeping your knee bent for long periods while working or driving can increase your knee stiffness and pain. Avoid high heels. Wear appropriate footwear with cushioned soles or insoles.
Other options
Some people find purchasing a Transcutaneous Electrical Nerve Stimulator (TENS) machine, insoles or cushioned footwear are helpful. The evidence for these, however, is somewhat limited. Similarly, some people find supplements such as glucosamine or chondroitin are helpful, especially in the early stages. Again, there is limited evidence for these. There is, however, no evidence that these other options are harmful, provided you have no other medical conditions. It is best to ask your healthcare professional or pharmacist before using any of these.
Some people find that they can also get some pain relief from using hot or cold packs. Try wrapping crushed ice in a damp towel and hold it for ten to fifteen minutes against the part of the knee that hurts. You can do this every two to three hours. Make sure you use a damp towel between the ice and the skin to avoid an ice burn.
You could also use a heat pad or a hot water bottle with an insulated cover on it. Make sure this is not too hot and not directly touching your skin. You can apply this for ten to fifteen minutes three to four times a day.
Medication
If you still have pain after trying the above you can speak to your doctor who may discuss medication for pain relief. There are several different types of pain relief that your doctor can prescribe before thinking about having a knee replacement.
Surgery
You will not necessarily need a knee replacement if you have osteoarthritis of your knee. Your healthcare team will always try non-surgical measures first before suggesting a knee replacement. If your symptoms are still manageable and your pain medication is effective then you may prefer to wait and continue without surgery. Most people who have a knee replacement are over 55. One of the reasons for this is that the earlier you have a knee replacement the greater the chances that you will eventually need further surgery on the same knee because the implant wears out and needs to be replaced again. There is also evidence that the younger patients are more likely to be unhappy with their knee replacement. This “re-do” procedure is called revision knee surgery and it is more complex than doing your knee replacement for the first time. As a result revision knee surgery comes with potentially higher risks and complications.
What is a knee replacement and what risk are associated with it?
If your knee is damaged by arthritis and the pain, stiffness and disability are having a serious impact on your everyday activities and you have tried all the self help advice, we may offer you a knee replacement. Knee replacement surgery is performed in ultra-clean theatres by a highly trained team of surgeons anaesthetists-nurses and it is generally a very successful operation resulting in good pain relief and improved mobility. During the surgery a part of the knee or the total knee joint is replaced with an artificial joint.
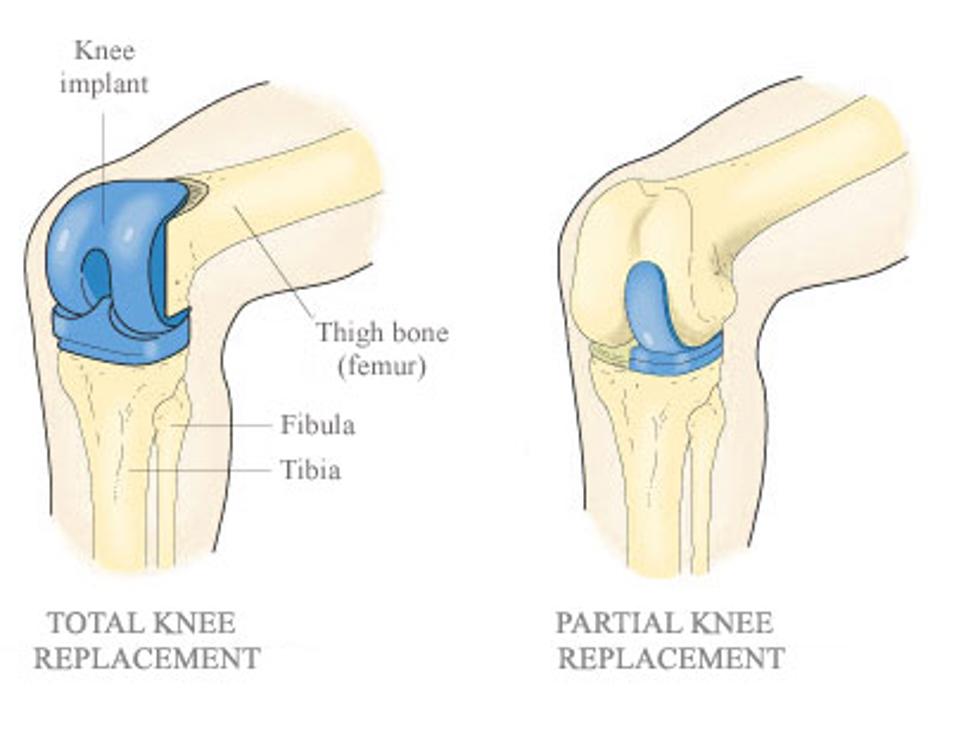
Figure 2: Schematic drawing of a total knee replacement and a partial knee replacement
What is a knee replacement and what risk are associated with it?
Unfortunately, some people may not be able to have a knee replacement even though their arthritis is very bad. It is important you are the best shape you can be prior to undergoing what is major surgery in order to ensure surgery is as safe as possible. Decisions about the timing of surgery will also consider the extent of the underlying knee arthritis. Possible reasons why surgery may not go ahead:
- You have a medical condition that puts you at too high a risk for either surgery or anaesthesia.
- If your body weight and body mass index (BMI) are too high (BMI greater than 40kgs/m2) or too low (BMI lower than 20kgs/m2). This may need to be addressed prior to surgery.
- If you are anaemic (too little iron in the blood) again this may need to be corrected prior to surgery.
- If you are diabetic and your diabetic control is poor this again may need to be corrected.
- Your thigh muscles (quadriceps) are very weak and may not be able to support your new knee joint.
- You have deep or long-lasting open sores (ulcers) in the skin below your knee or your leg circulation is poor. Both increase your risk of infection and wound problems.
Procedure
The knee is the largest weight bearing joint in the human body and as such it can be prone to ‘wearing out’. Arthritis is painful and disabling and you and your surgeon may have decided that a knee replacement may be your best option if all measures have failed.
A knee replacement is a surgical procedure, in which the injured or damaged weight-bearing surfaces of the knee are replaced with artificial parts, which are secured to the bone.
You will see the surgeon before your operation. They will take this opportunity to draw (mark with a pen) on your leg. This is to make sure they operate on the correct leg. If you have any questions, this is a good time to ask them.
Staff will give you an anaesthetic in the theatre. This may be a general anaesthetic (where you will be asleep) or a local block (e.g. where you are awake but the area to be operated is completely numbed). The anaesthetist will discuss this with you.
Staff may place a tight inflatable band (a tourniquet) across the top of the thigh to limit the bleeding. We will clean your skin with antiseptic solution and cover the area with clean towels (drapes). The surgeon will make an incision (a cut) down the front of the knee. The knee capsule (the tough, gristle-like tissue around the knee), which is then visible, can be cut and the knee cap (patella) pushed to one side. From here, the surgeon can trim the ends of the thigh bone (femur) and shin bone (tibia) using a special bone saw. Some surgeons also remove the underside of the knee cap.
Using measuring devices, the new artificial knee joints are fitted into position. Your new artificial knee joint will be made from a combination of very high-grade metal alloy fixed to the femur and tibia and a very high-grade plastic (polyethylene) bearing sandwiched in between the metal parts. Sometimes, the surgeon places a polyethylene button on the underside of the knee cap.
When the surgeon is happy with the position and movements of the knee, they will close the tissue and skin. They may use stitches (sutures) or metal clips (skin staples). The clips and stitches will need to be removed around 10 to 12 days after the operation.
Drains may occasionally be used, and if so, these can be pulled out easily on the ward in a day or two.
When you wake up, you may have a bandage around the knee. If you are in pain, please ask for pain killers. If you have pain, it is important that you tell the ward staff.
You will go for an X-ray the day after the operation and we will encourage you to stand and take a few steps either on the day of surgery or the latest the next day after the operation.
You will be in hospital for as long as it takes for your pain to be under control and for you to be safe walking with crutches. This usually will only be a day or two at most and may even be the same day as you have your operation. Occasionally patients stay in longer than this.
The physiotherapy team will visit you, and suggest exercises for you. It is important to do these (as pain allows).
Please be aware that the surgeon who carries out your operation may either be your consultant or another surgeon who is well trained and/or supervised to perform your knee replacement.
Risks
As with all surgical procedures, knee replacement carries some risks and complications:
- Pain: Your knee will usually be sore for a few days/weeks after the operation. If you are in pain, it’s important to tell ward staff so they can give you medicines. Pain will improve with time. Rarely, pain will be a chronic or long-term problem and may be due to any of the other complications listed below or for no obvious reason.
- Dissatisfaction: The majority of patients are satisfied following knee replacement surgery, however, up to 15% to 20% of patients may experience some discomfort in their knee and may not be entirely satisfied with their knee replacement and up to 5% may feel that they are worse off.
- Kneeling: Even though it is safe to kneel on your replaced knee (once the wound has fully healed) around half of patients find it uncomfortable to kneel after having their knee replaced.
Other Common Risks: (2% to 5%)
- Bleeding: Some patients may occasionally need a blood transfusion or iron tablets. Rarely the bleeding may form a blood clot or large bruise within the knee, which may become painful and may require an operation to remove it.
- Deep Vein Thrombosis (DVT): Is a blood clot in a vein. The risks of developing a DVT are greater after any operation (and especially a bone operation). A DVT can pass in the blood stream and be deposited in the lungs (a pulmonary embolism (PE) or in your brain (a stroke). These are less common, but very serious conditions. Your surgeon may give you medication to try and limit the risk of DVTs from forming. Some hospitals will also ask you to wear stockings on your legs, while others may use foot pumps to keep blood circulating around the leg. Starting to walk and moving about as soon as possible after your operation is one of the best ways to prevent blood clots from forming.
The risks of DVT are increased in certain types of patients such as those with a family history of clots, those with other serious diseases such a kidney or liver disease and obesity. The biggest risk factors that you can do something about are obesity and smoking and you should try and address these before you even consider a knee joint replacement if you are overweight or smoke. This will significantly reduce your risk of clots.
- Knee stiffness: Stiffness of the knee may occur after the operation, especially if the knee is stiff before the operation. Manipulation of the joint (under general anaesthetic) may be necessary.
- Prosthesis wear: With modern operating techniques and new implants, knee replacements last many years. In some cases, however, they may fail earlier. The reason is often unknown. The plastic bearing is the most commonly worn away part. When the replacement wears out or loosens it will become painful again and more surgery may be required. With newer designs of replacements however, wear is becoming less of a problem than it was in the past. Overall, around 96% of total knee replacements and 87% of partial knee replacements will last at least 15 years.
Less Common Risks: (1% to 2%)
- Infection: We will give you antibiotics at the time of the operation and the procedure will also be performed in sterile conditions (theatre) with sterile equipment. Despite all these preventative measures, infection can still occur (up to 1% to 2%). The wound site may become red, hot and painful. There may also be a discharge of fluid or pus. We usually treat this with antibiotics and an operation to washout the joint may be necessary. In rare cases, the prosthesis may be removed and replaced at a later date. The infection can sometimes lead to sepsis (blood infection) and strong antibiotics are required in addition to further surgery.
Illnesses or medication that weakens the immune system such as diabetes, rheumatoid arthritis or immunosuppressant drugs increase the risk of infection as does obesity.
The biggest risk factors that you can do something about are obesity and smoking and you should try and address these before you even consider a knee joint replacement if you are overweight or smoke. This will significantly reduce your risk of infection.
If you are diabetic then having good control of your sugar levels (HbA1c levels <7) will again significantly reduce you risks of developing an infection following surgery.
- The risks of infection after a unicompartmental or partial knee replacement are around half that of a total knee replacement.
Rare Risks: (less than 1%)
- Pulmonary Embolism (PE): is the spread of a blood clot to the lungs and can affect your breathing. This can be fatal.
- Altered wound healing: the wound may become red, thickened and painful (keloid scar), this is especially prevalent in Afro-Caribbean’s.
- Joint dislocation: if this occurs, the joint can usually be put back into place without an operation. Sometimes this is not possible, and an operation is required, followed by application of a knee brace. If your knee replacement remains unstable, further revision surgery may be required.
Occasionally knee replacements with mobile or floating bearings are used and rarely these bearings can dislocate and require surgery to put back in place.
- Nerve Damage: efforts are made to prevent this; however there is a risk of damage to the small nerves of the knee. This may cause temporary or permanent altered sensation around the knee. There may also be damage to the Peroneal Nerve, this may cause temporary or permanent weakness or altered sensation of the lower leg. Changed sensation or numbness to the outer half of the knee next to the incision is very common and usually improves, at least partially, over time.
- Bone Damage: bone may be broken when the prosthesis (artificial joint) is inserted. This may require fixing either during the operation or at a later date.
- Blood vessel damage: the vessels at the back of the knee may rarely be damaged, this may need another operation. Your risks of permanent and serious damage to the vessels behind the knee are increased if you already have circulation problems or have had previous surgery to this area.
- Death: This very rare complication may occur after any major operation and from any of the above. Overall, the risk of dying after a knee replacement is very low, but death does occur in around 1:1000 patients. The risks of dying after a unicompartmental or partial knee replacement are around half that of a total knee replacement.
Further Useful Information
|
Versus Arthritis: |
https://versusarthritis.org/about-arthritis/conditions/osteoarthritis-of-the-knee/
|
|
Hip and Knee Replacement General Advice: |
www.youtube.com/watch?v=xAL_TrQdtTY
|
|
General Persistent Pain Advice: |
https://youtu.be/C_3phB93rvI?si=rO7a24gN1HtKoVBd
|
|
Fife Sport and Leisure: |
This leaflet has been reviewed by patients and staff of NHS Fife.
Appendix 1
Useful Exercises:
These exercises can be undertaken on the affected side(s) and alternated. The repetitions and sets given are for guidance only and can be adjusted depending on pain levels.

1. Knee Slides
Sit with a towel under one foot.
Bend and straighten your knee by sliding your foot along the floor or on a smooth piece of board on your bed.
Alternately you can do this in sitting whilst sliding the foot along the floor

2. Thigh Sets (strengthening)
Tighten the muscles at the front of your thigh. Bend your ankle and push your knee down firmly against the bed or floor and hold that position.
Repetitions = x10 repeats
Number of Sets = 1 to 3 sets
Seconds (Secs) hold time = 5 to 10 seconds holds
Daily = once to three times a day

3. Short Arc Thigh Sets (strengthening)
Lying on top of a bed (or on the floor if able), bend one knee over a pillow or rolled up towel. Straighten your lower leg keeping the back of the knee in contact with the pillow or rolled up towel. To make the exercise harder put a weight around your ankle being raised.
Reps = x10
Sets = 1 to 3
Secs = 5 to 10 second holds
Daily = once to three times a day


4. Sitting Thigh Holds (strengthening)
Pull your toes up, straighten your knee and tighten your front thigh muscles. Hold the ‘straight’ position and then slowly lower your leg.
Reps = x10
Sets = 1 to 3 Secs = 5 to 10 second holds
Daily = once to three times a day

5a. Knee Stretches
Rest you heel on a rolled towel or cushion.
Let the weight of your leg gently straighten your knee then hold the stretch

5b. Knee Stretches
If managing Exercise 5a easily progress to:
Sitting with one leg supported on another chair, lean forward from the hips keeping your back straight. Straighten your knee assisting the stretch with your hands and hold.
Reps = x10
Sets = 1 to 3
Secs = 5 to 10 second holds
Daily = once to three times a day
A more prolonged stretch, approximately 5 to 10 minutes can be achieved by moving the ‘supporting leg chair’ slightly further out so that just the foot and ankle are supported. Allow the back of the knee to stretch downwards under the effect of gravity as you are sitting. Repeat once or twice a day, instead of or in addition to the exercises above, if able.

5c. Knee Stretches
Or
Standing with foot on a slightly raised surface lean forward from the hips keeping your back straight. Straighten the knee, assisting the stretch with your hands and hold.
Reps = x10
Sets = 1 to 3
Secs = 5 to 10 second holds
Daily = once to three times a day


6. Knee Bend Stretching
Standing and holding onto the back of a chair, bend your knee behind you and lift your foot/heel off the floor towards the ceiling.
Reps = x10
Sets = 1 to 3
Secs = 5 to 10 second holds
Daily = once to three times a day
Aerobic Exercises
These exercises are best combined with aerobic exercises i.e. exercises that work the heart and lungs such as walking or cycling (or exercises in a swimming pool, if able).
If your symptoms do not improve within 6 weeks of doing these exercises you may want to seek advice from a physiotherapist.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
