Introduction
The purpose of this leaflet is to provide you information about knee osteoarthritis and how to best manage it, especially in situations where knee replacement surgery is not currently indicated or feasible.
What is knee osteoarthritis (OA)?
Osteoarthritis is the most common form of arthritis and the knee is a commonly affected joint. A joint is a part of the body where two bones meet. The ends of the bones in a joint are covered in a smooth and slippery surface known as cartilage. This allows the bones to move easily against each other and protects the bones from stress. In the knee there is a joint between the thigh and shin bones as well as a small joint between your patella and the thigh bone.
Osteoarthritis causes the cartilage in your knee joint to thin and the surfaces of the joint to become rougher, which means that the knee does not move as smoothly as it should (Figure 1).
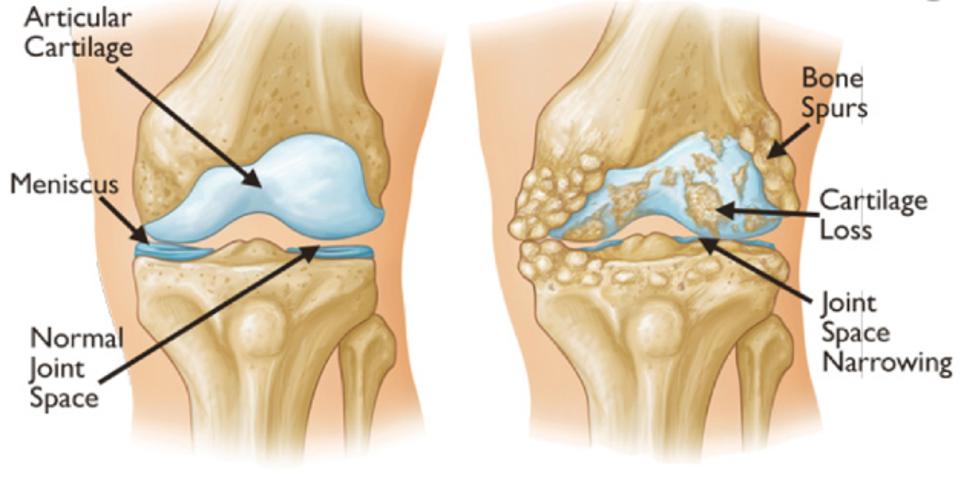
Figure 1 The drawing on the left hand shows the typical appearance of a healthy knee joint, and the right hand side is an arthritic knee joint
What are the symptoms?
These vary from person to person and you may experience:
- Pain around the knee joint.
- Stiffness
- Swelling
- Difficulty doing tasks or activities.
- Weakening of the muscles
What are the causes?
Joints go through a normal cycle of damage and repair during our lifetime. Sometimes the body’s process to repair our joints can cause changes in their shape or structure. When these changes happen it is known as osteoarthritis.
Osteoarthritis is more common in people over the age of 50. Women tend to be more affected by knee osteoarthritis than men. Previous injury such as fractures or surgery can lead to osteoarthritis developing. Being overweight is also linked to osteoarthritis especially in large weight bearing joints such as the knee.
How is it diagnosed?
Knee Osteoarthritis is diagnosed through a clinical examination and by signs and symptoms reported by you. An x-ray may be used to confirm and assess the changes in the knee.
Should I have an x-ray or scans?
An x-ray is commonly used to assess knee osteoarthritis. A Magnetic Resonance Imaging (MRI) scan is not normally required.
What is the prognosis?
Most people will experience ongoing symptoms. However a diagnosis of knee osteoarthritis does not necessarily mean a continued deterioration in the joint or progressive pain. It is also important to note that changes on an x-ray may not correlate with the pain that a person may experience.
Self-care, advice and exercise should help you cope with and manage your symptoms. It will often take around 3 to 6 month of exercise participation to see improvement
Is knee osteoarthritis serious?
Knee Osteoarthritis can be very painful and affect your ability to take part in activities but is not usually serious.
What are the treatment options?
There is strong evidence that exercise may benefit symptoms of osteoarthritis. Joints need to move and exercise to keep them healthy. Whatever your fitness level, exercise can help the knee to be able to cope with normal daily activities.
If pain is a problem consult your GP or pharmacist to get advice on pain medication.
Depending on your past medical history, your GP may prescribe Non-steroidal Anti-Inflammatory Drugs (NSAIDs).
Your GP or health professional may suggest a knee joint injection. This is a corticosteroid injection which may help to reduce pain and inflammation in your knee.
If symptoms have become unmanageable then surgery may be an option. You would be referred to an Orthopaedic Surgeon but your GP or health profession to discuss any surgical options.
What can I do myself to help manage my symptoms?
Advice to help improve symptoms:
- Try to remain active and stay at work even if you have to modify your duties.
- Strengthening and stretching the muscles which support the ankle, knee, hip and back.
- Going for walks, cycling or swimming can also help reduce pain and improve your mobility and general health.
- Weight loss decreases the load on the joints and has been shown to significantly reduce pain.
- Applying a hot pack or ice packs can help with pain and swelling for 5 to 10 minutes two to three times a day. Make sure you place a damp towel between the ice and your skin to prevent an ice burn. Further information can be found on the NHS Inform website
How can physiotherapy help?
Your Physiotherapist will provide a programme of exercises to help maintain your knee range of movement and build up the muscle strength around your knee.
Sometimes you may experience an increase in your pain, with or without warning. If you experience flare-ups, you need to reduce your day to day activities and frequency/intensity of physiotherapy exercises to lessen the overall load placed on the knee. Most people recover quickly from flare-ups by pacing, activity modification and by taking appropriate painkillers. It is also vital you provide adequate time for the muscles to recover and do not push through the pain and avoid sudden increase in the intensity of the exercises.
It is very important that you have an active role in the management of your condition and work with your physiotherapist to help improve your condition.
How often should I do these exercises?
Stretching
There is no exact stretching time that works for everyone. Current evidence suggests stretching for 30 to 60 seconds in total may be optimal. This could be one or two sets of 30 second holds or three sets of 20 seconds.
It is, however, best to start with one or two stretches held for 10 seconds or so and gradually build this up to between 30 and 60 seconds. Stretching can feel uncomfortable, but should not feel painful during or after the exercise.
Rehabilitation Exercises
Try to do these exercises once a day on the majority of days. It is important to have rest days, especially if you are not used to exercising regularly. It is acceptable to break the exercises into groups and complete these at different times in the day.
Start with one set of 5 to 10 repetitions. As the exercise becomes easier you can either gradually increase the repetitions or add another set of exercises. A total of 45 repetitions would be a maximal effort i.e. 3 sets of 15 repetitions. Take a rest of up to a minute between each set. Ideally the muscle(s) you are exercising should begin to feel fatigued by the end of the exercise however you should not be straining. It is normal to have some discomfort during exercises as long as it’s acceptable to you.
As you increase the repetition of exercises you should try to have a rest day after each exercise day to allow your muscles to recover.
Rehabilitation Exercises
Aims:
- Minimise pain and swelling
- Regain full range of movement of the knee
- Increase muscle strength.
- Restoration of normal walking pattern
Rehabilitation Exercises

1. Knee Slides
Sit with a towel under one foot.
Bend and straighten your knee by sliding your foot along the floor or on a smooth piece of board on your bed.
Alternately you can do this in sitting whilst sliding the foot along the floor.

2. Knee Extension
Rest you heel on a rolled towel or cushion.
Let the weight of your leg gently straighten your knee then hold the stretch.

3. Inner range quads
Lying on your back. Bend one leg and put your foot on the bed and put a cushion under the other knee.
Exercise your straight leg by pulling your foot and toes up, tightening your thigh muscle and straightening the knee (keep knee on the cushion).


4. Straight Leg Raise
Lie on your back with one knee bent keeping your back flat on the bed.
Tighten your front thigh muscles and lift the straight leg. Lower the leg to the starting position in a controlled manner.

5. Side-lying Hip Abduction
Lie on your side with your upper leg straight.
Lift your upper leg as far as you can, without letting your pelvis rotate backwards.


6. Mini-squat with support
Stand and take support if needed.
Squat down and at the same time move your pelvis slightly backwards. Straighten your hips and return to the starting position.

7. Knee Extension in Sitting
Sit up straight on a sturdy chair, so that your feet are supported on the floor.
Bend your ankle and straighten your knee using your front thigh muscles.
In a controlled manner, return to the starting position.
Rehabilitation Exercise Progression
Criteria for exercise progression
- Minimal or no pain
- Minimal or no swelling
- Good knee joint range of movement.
- Rehabilitation exercises feeling easy.
Aims
- Improve muscle strength
- Improve range of motion and flexibility
- Improve exercise tolerance


1. Bridge
Lie on your back with legs bent.
Squeeze your buttock muscles and roll your pelvis off the floor.
In a controlled manner, return to the starting position.

2. Sit to Stand
Sitting with your arms crossed.
Stand up and then sit down slowly on a chair. (This can be made easier and more difficult by changing the height of the chair)



3. Step Ups
Stand tall behind a step and take support, if needed.
Place your whole foot on the step and step up.
Note: While stepping up keep hip, knee and toes aligned.

4. Single-leg Standing
Balance on one leg.
(Ensuring your safety at all times if your balance is poor).
Remember to stand tall, with weight evenly on your foot and toes pointing forwards.
Perform 2 to 3 repetitions 20 to 30 seconds as able.

5. Standing Hamstring Stretch
Stand with the leg to be stretched on a footstool.
Bend your ankle up towards your body and push the heel towards the footstool keeping your knee straight.
Then bend your upper body forwards from your hips keeping your back straight. You should feel the stretching behind your knee and thigh.

6. Side Lying Quadriceps Stretch
Lie on your side with your knees bent. Put a towel around your top ankle.
Hold the towel and pull the ankle towards your buttock.
Tighten the buttock muscles and straighten your hip. Do not arch your back.

7. Calf Stretch
Stand with your feet hip width apart and take a step forward.
Take most of your weight on the front foot. Gradually take your weight to the back foot stretching your heel to the floor. Keep your back in line with your back leg.
Getting back to normal
Returning to activities of daily living
There are no specific timeframes regarding when you can return to activities of daily living. It is advised that you aim to gradually build up the exercises in this leaflet and then gradually return to activities as able. It is advised that you use the same guidelines regarding discomfort as for the exercises, i.e. discomfort should be at a level you consider to be manageable and should settle within 24hrs.
Guidance for returning to work
Research suggests that staying active and keeping moving as pain allows, will help you get better sooner. Getting back to work helps most people with back pain. If you are ‘signed-off’ work, time frames for returning to work will depend on the type of work you do and a healthcare professional can advise on this. It is advised you communicate regularly with your employer to facilitate a safe and timely return to work.
Useful Information
|
Information |
Link |
|
NHS Inform |
www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints |
|
NHS Inform – How to Apply ICE |
|
|
The Chartered Society of Physiotherapy |
www.csp.org.uk/conditions/managing-your-bone-joint-or-muscle-pain |
|
Versus Arthritis |
|
|
Escape Pain |
Worries or concerns
Should you have any worries or concerns, please contact your GP during working hours or contact NHS24 on 111 out of working hours.
If you continue to experience problems then you should consult a healthcare professional.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
