Fife Musculoskeletal Physiotherapy
This information has been developed to supplement the information the Doctor or Healthcare Practitioner has already given you.
Issue No: 4.2.3.5.14.1
Date of Issue: February 2025
Review Date: February 2026
If the review date has passed, the content will apply until the next version is published.
Introduction
The information provided describes the situation where one of the meniscus (sometimes referred to as the cartilages) has become irritated. This is common and can occur during the normal wear and repair processes at the knee. The information will outline how best to manage your symptoms should you suffer a flare-up.
What is Meniscal Degeneration of the knee?
The menisci are C-shaped tissues (cartilage) inside the knee joint, located between the thigh (femoral) and shin (tibia) surfaces. There is one on the inside of the joint (medial) and one on the outside (lateral) (Figure 1).
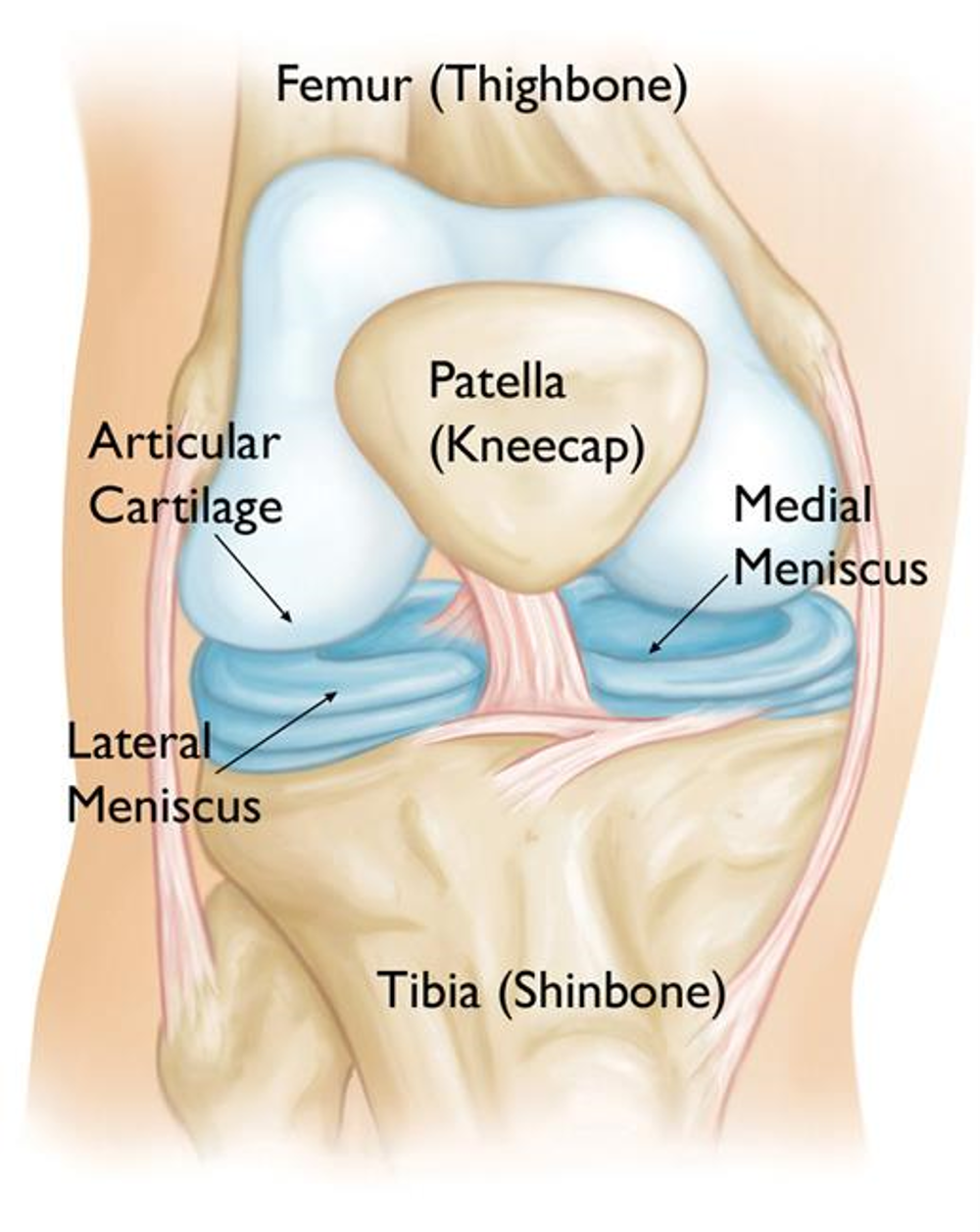
Figure 1: Front view of the right knee joint
The menisci (cartilages) have several important functions:
- increasing knee joint stability
- joint lubrication
- helping balance
- shock absorption.
Normal wear and tear was sometimes previously called ‘degeneration’. It is now known that the menisci undergo different processes during their life time and can wear, but also recover, hence the term wear and repair is more appropriate.
What are the symptoms?
These vary from person to person. People may experience:
- Pain
- Swelling
- Giving way
- Reduced function of the knee (the inability to straighten the knee or locking)
What are the causes?
There is no one specific cause of irritated menisci. They are probably an early sign of osteoarthritis (the normal ageing process of joints), rather than a completely separate diagnosis. Many middle-aged and older people have evidence of meniscal wear and repair without knee pain.
Should I have an x-ray or scans?
Knee scans are usually done for knees where there is significant ligament damage and surgery may be required. They are not useful in the case of meniscal wear and repair changes as they cannot tell us where the pain is.
An x-ray may be useful if you have completed some rehabilitation, but you are still struggling with pain.
What is the prognosis?
This condition often takes 3 to 6 months of rehabilitation to settle or see improvement.
It is normal to have flare ups during this time. If this happens, then it may be best to reduce the repetitions or rest for a few days before starting again.
Treatment
The main principles when gradually rehabilitating your knee are:
- Control pain and swelling
- Gradually restore full range of motion
- Improve muscle strength and joint stability
- Improve your balance and co-ordination
- Improve your general cardiovascular (aerobic) fitness.
What can I do myself to help?
Medication: Use medication to manage your pain and help stay active in the short term. It is recommended you take your medication regularly at the prescribed dose rather than wait until the pain is at its worst. It is best to speak to your GP, pharmacist or a suitably qualified healthcare professional about which medication is best to take for your particular symptoms.
Pacing and modifying activity: This is about keeping your pain and symptoms under control. You may want to avoid or decrease the activities that cause your knee pain.
You may have ‘flare-ups. Pacing can be achieved by following a simple traffic light system:
- Green – Pain is manageable, continue your chosen activity
- Amber – Pain is increasing, reduce your chosen activity
- Red – Pain is at high level, too much activity too soon and you need to minimise your chosen activity.
It is important not to ‘push through’ the pain.
Ice Packs: Apply an ice pack for 5 to 10 minutes two to three times a day. Make sure you place a damp tea towel between the ice and your skin to prevent an ice burn. Further information can be found on the NHS inform website
Avoid Smoking: Smoking increases the sensitivity of nerves which can lower your pain threshold and thus increase your pain levels. Smoking can slow down recovery and increase the release of stress hormones. Smoking can put you at risk of other adverse health conditions.
Please visit www.nhsinform.scot/healthy-living/stopping-smoking for more information or get in touch with your GP if you require assistance to stop smoking.
How can physiotherapy help?
Your physiotherapist will provide a specific exercise programme which will assist you through the different stages of recovery. Your initial exercises will be aimed at reducing your symptoms and improving your range of movement at your knee.
It is important to note that these exercises should not aggravate your symptoms. You are advised to stop the exercises and contact your physiotherapist if you are not able to tolerate the exercises suggested. Your physiotherapist will be able to advise you on alternative techniques or other activities.
It is important that you play an active role in the care of your condition to aid recovery.
Following the exercises are just suggestions that some patients have found helpful in the past. Unfortunately, there are no exercises that suit everyone.
If you follow the exercises below and experience an increase in your symptoms, please reduce the range of movement and the number of repetitions or sets. Gradually increase these as your symptoms allow. You may need to leave it for 24 to 48 hours before trying again.
Rehabilitation exercises
Aims:
- Maintain and gradually restore range of knee movement.
- Maintain and gradually restore muscle activity around your knee and hip.
How often should I do these exercises?
Stretching
There is no exact stretching time that works for everyone. Current evidence suggests stretching for 30 to 60 seconds in total may be optimal. This could be one or two sets of 30 second holds or three sets of 20 seconds.
It is, however, best to start with one or two stretches held for 10 seconds or so and gradually build this up to between 30 and 60 seconds. Stretching can feel uncomfortable, but should not feel painful during or after the exercise.
Rehabilitation exercises
Try to do these exercises once a day on the majority of days. It is important to have rest days, especially if you are not used to exercising regularly. It is acceptable to break the exercises into groups and complete these at different times in the day.
Start with one set of 5 to 10 repetitions. As the exercise becomes easier you can either gradually increase the repetitions or add another set of exercises. A total of 45 repetitions would be a maximal effort i.e. 3 sets of 15 repetitions. Take a rest of up to a minute between each set. Ideally the muscle(s) you are exercising should begin to feel fatigued by the end of the exercise however you should not be straining. It is normal to have some discomfort during exercises as long as it’s acceptable to you.
As you increase the repetition of exercises you should try to have a rest day after each exercise day to allow your muscles to recover.
Rehabilitation Exercises
The initial goal of early treatment is to help settle your pain/swelling.

1. Simple knee bends
Sitting with the legs straight or with the non injured leg over the edge of a bed. Bend your injured knee by sliding the heel up and down along the floor. Ideally you would want to do this on a smooth floor or surface such as a tray.
Repetitions: 10 times.
Sets: 3 sets at a time
Daily: Repeat every 1 to 2 hours during the daytime.

2. Knee bend stretches
Long sitting. Put a towel around your foot.
Bend your knee as far as possible. Gently pull the towel to bend your knee a little more.

3. Heel slides
Sit on a chair with the foot on a smooth floor and or towel under one foot.
Slide the foot under the chair as far as you can. Move your knee forward keeping the sole of your foot in contact with the floor.

4. Knee straightening
Place a rolled towel under your ankle.
Straighten your knee by tightening your thigh muscles. Try to touch the floor with the back of your knee.

5. Sitting knee extension
Long sitting place a rolled up towel under your knee.
Pull your toes up, tighten the front of your thigh muscle and straighten your knee slowly lifting your foot up.

6. Lying
Lying on your back. Push your knee down onto the bed and lift your foot up off the floor/bed.

7. Standing small knee bends
Standing tall, with your feet hip width apart. Gently bend both knees as if you are going to sit down. Hold this position for a few seconds then straighten your knees by squeezing your front thigh muscles and your buttock muscles.
Rehabilitation exercise progression
Criteria for Progression:
- Minimal or no pain
- Minimal or no swelling
- Good range of movement
- Minimal symptoms with previous exercises.
Aims:
- Improve range of movement
- Improve strength
- Restore function.

1. Hamstring stretches
Sit on a sofa with one leg straight in front of you with the heel over the edge and the other leg on the floor (as shown).
Bend your upper body forwards keeping your back straight.

2. Thigh muscle quadricep stretches
Lying on your side with your legs bent. Take hold of the ankle of your upper leg. Gently draw your foot towards your buttock. Feel the stretch in the front of your thigh.

3. Sit to stand
Sitting with your arms crossed.
Stand up and then sit down slowly on a chair. (This can be made easier and more difficult by changing the height of the chair).

4. Single leg balance
Stand on one leg.
Hold for 30 seconds.
Repeat 3 times

5. Step ups
Stand on a step.
Bend one knee and straighten your other leg behind you.
Do not let the bent knee turn in or out at any point in the movement. Return to the starting position.

6. Single step downs
Stand on one leg on a step facing down.
Slowly lower yourself by bending your knee to 30 degrees.
Return to starting position.

7. Static bike
Exercise bike (if available).
10 to 15 minutes of moderate resistance.
Note: If any of these activities or exercises increase your knee pain or symptoms, please stop the activity or exercise until you have discussed them with our physiotherapist or doctor.
Getting back to normal
Returning to activities of daily living
There are no specific time frames for returning to your usual activities and these vary from person to person. Symptoms may be ongoing for several months and you may need to adjust your activities and pace yourself during your recovery. Aim to increase your levels of activity gradually, avoiding worsening of your symptoms. Progress your activities as your symptoms and movements improve.
It is advisable to take regular breaks if sitting or driving for long periods of times.
Guidance for returning to work
Research suggests that staying active and keeping moving as pain allows, will help you get better sooner. Getting back to work helps most people with back pain. If you are ‘signed-off’ work, time frames for returning to work will depend on the type of work you do and a healthcare professional can advise on this. It is advised you communicate regularly with your employer to facilitate a safe and timely return to work.
Useful Information
NHS Inform
www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints
The Chartered Society of Physiotherapy
www.csp.org.uk/conditions/managing-your-bone-joint-or-muscle-pain
Worries or concerns
Should you have any worries or concerns, please contact your Physiotherapist or GP during working hours or contact NHS24 on 111 out of working hours.
If you continue to experience problems then you should consult a healthcare professional.
Diagram: Static Bike Diagram Courtesy of previous ©PhysioTools
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
