Fife Musculoskeletal Physiotherapy
This information has been developed to supplement the information the Doctor or Healthcare Practitioner has already given you.
Issue No: 4.1.3.5.1
Date of Issue: February 2025
Review Date: February 2026
If the review date has passed, the content will apply until the next version is published.
Introduction
This leaflet will provide you with information about neck (cervical) nerve root pain and how to manage your symptoms.
What is Cervical Nerve Root Pain?
Cervical nerve root pain (or radiculopathy as it is sometimes termed) is a neck condition that causes compression or irritation of the nerves that supply the shoulders, arms and hands. It usually affects only one side, but it can more rarely affect both sides.
What are the symptoms?
Common symptoms are neck pain, pain in the shoulder blades and pain radiating to the arm and sometimes into the hand. Depending on the severity of the problem, you may also experience heaviness, weakness and tingling sensation of the affected arm/hand.
What are the causes?
To understand some of the causes, it is worth looking at the basic structure of the spine (Figure 1).
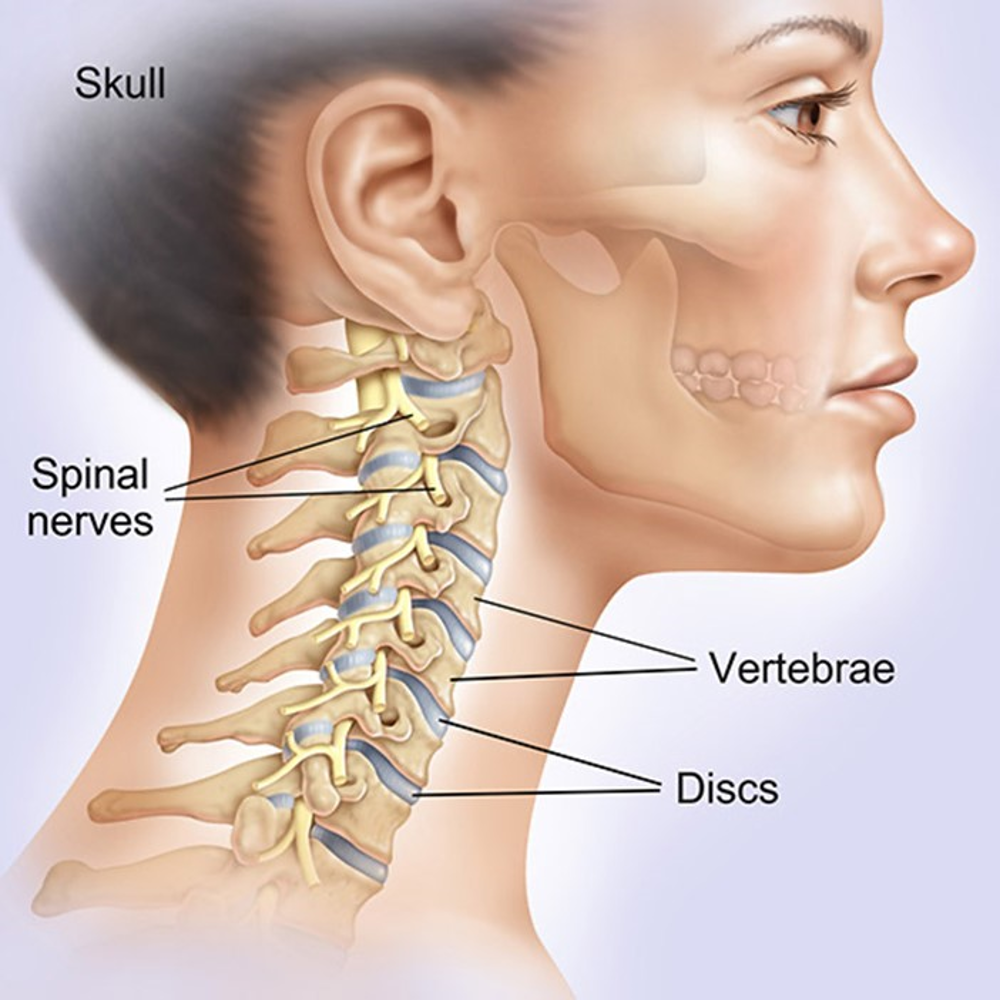
Figure 1 - Anatomy of the spine.
The spine is made up of various different parts, including:
Vertebrae – bones which are stacked to make up the spinal column. Each vertebra consists of a solid body forming the front of the column and loop-shaped bone at the rear. Together these form a channel which houses and protects the spinal cord/nerves.
Spinal cord and nerve roots – The spinal cord is the main band of nerves which connects the brain to the rest of the body and sits in the channel formed by the vertebrae. Spinal nerves that connect to your limbs and organs branch out from the spinal cord between each of the vertebrae. Where these nerves attach to the spinal cord is known as the nerve root.
Discs – The discs in between each of the vertebrae provide shock absorption and allow movement of the spine. The discs have a tough outer layer and a gel-like centre.
Muscles, tendons, and ligaments – are known as ‘soft tissues’. These connect the bony structures and support the spine.
Cervical nerve root pain can occur when changes in the spine causes a nerve or nerves to become compressed or irritated.
Some examples include:
- A disc between the vertebrae can ‘bulge’ due to age, repetitive movements or injury. This occasionally causes it to irritate or press on a nerve in the neck. (A spinal disc which ‘bulges’ is also sometimes called a ‘herniated’ or ‘prolapsed’ disc).
- Age-related wear and repair changes are part of normal aging. Occasionally the small spinal joints can become thickened and swollen, compressing and irritating a specific nerve.
When a nerve root is irritated you may feel symptoms in your upper limbs and sometimes the neck. The symptoms in the arm are the result of the areas supplied by these nerves being irritated in the neck. These arm symptoms e.g. pain, pins and needles (tingling) and or numbness are often known as ‘referred’ pain or symptoms.
Depending on the nerve root affected you may feel symptoms in different patterns of referred pain. These patterns may help your healthcare professional identify where the symptoms originate (Figure 2).
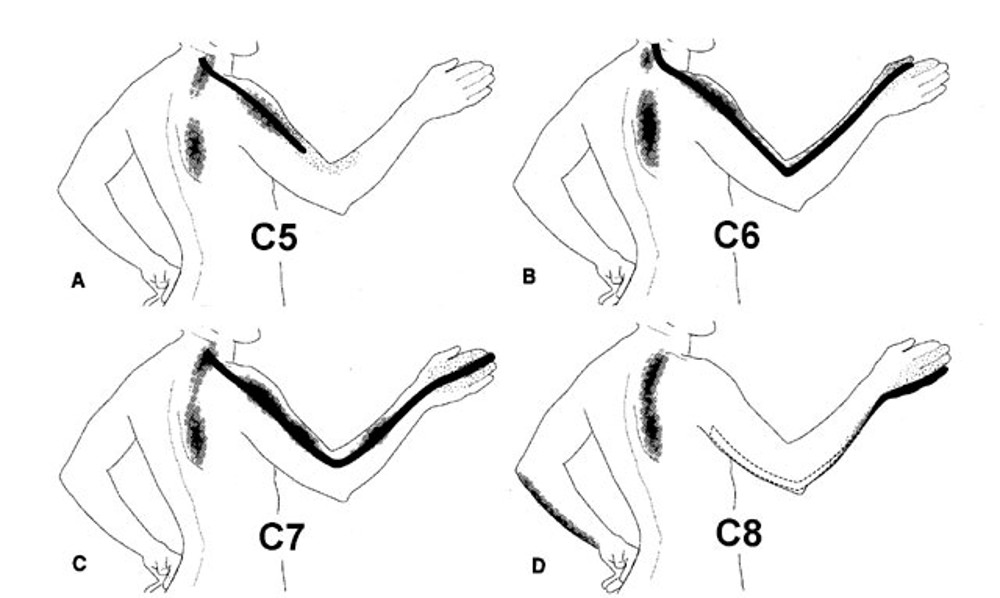
Cervical referred pain patterns depending on nerve affected (C number)
Management Advice Post Surgery
How is it diagnosed?
Cervical nerve root pain is diagnosed through a clinical examination and by the signs and symptoms you report.
Should I have an x-ray or scans?
An x-ray or scan of your spine may not help identify the cause of your symptoms unless there has been a direct injury. The spinal cord, nerves, discs, muscles, tendons or ligaments are not visible on x-ray.
A Magnetic Resonance Imaging (MRI) scan is not required in the early stages of cervical nerve root pain. Sometimes an MRI scan is requested if there are no signs of improvement. It is, however, important to note that most people recover within 3 to 6 months. Discuss with your doctor or physiotherapist if you feel you are not progressing as well as you would expect.
What is the prognosis?
Seventy five percent of patients will see some improvement within 4 to 6 weeks. Some people can experience mild and ongoing symptoms for several months.
Do not panic if you have a flare-up of your pain as small setbacks during the healing period are quite common. It may take up to 6 to 12 months for symptoms to fully settle. Occasionally symptoms may recur.
Self-care, advice and exercise should help you cope with your symptoms and aid recovery.
Is Cervical Nerve Root Pain Serious?
Cervical nerve root pain can be very painful, but is not usually serious. On rare occasions you may need to seek healthcare professional advice for your neck and arm pain if you have neurological symptoms such as:
- Vertigo (sensation that you, or the environment around you, is moving or spinning).
- Changes to eyesight (e.g. double or blurred vision).
- Difficulty in speaking or swallowing.
- Metallic taste in the mouth.
- Numbness of your face.
- Weakness of your face or limbs.
- Severe headaches.
Myelopathy is a rare condition resulting from compression of the spinal cord in your neck. Symptoms of myelopathy include:
- Having pins and needles or numbness on both sides in your hands or feet.
- Loss of dexterity (control in performing fine hand tasks), arm/hand weakness and control of the arm or legs.
- Walking with legs wider apart than normal (broad based gait/walking).
- Loss of bladder and/or bowel control.
Although very rare, it is important to treat these symptoms as an emergency. If you think you are experiencing symptoms of myelopathy you should seek urgent medical advice by calling NHS 111.
Treatment
What can I do myself to help cervical nerve root pain?
Medication: Use medication to manage your pain and help stay active. It is recommended you take your medication regularly at the prescribed dose rather than wait until the pain is at its worst. It is best to speak to your GP, pharmacist or a suitably qualified healthcare professional about which medication is best to take for your particular symptoms.
Positions of Comfort: You will know which pain-relieving positions work best for you (See page 8 for some suggestions).
Staying Active: Activity and exercise can seem daunting when in pain but it is one of the most effective tools in the management of your symptoms. Whilst a few days rest may be beneficial in the early stages, research has shown that prolonged rest is not helpful. Staying gently active without aggravating your symptoms will aid in your recovery.
Relaxation: Experiencing pain is complex and individual to each person. Many people report feeling increased levels of frustration, stress and low mood. This in turn can make your pain feel worse. You may wish to consider relaxation techniques such as Mindfulness, Tai Chi, or simple controlled breathing exercises. Please visit www.moodcafe.co.uk if you wish to explore various other self-care strategies to improve your mental health.
Sleep Pattern: Ensuring good sleep is essential. Please contact your GP if your pain is worse at night. Please see www.nhsinform.scot/illnesses-and-conditions/mental-health/mental-health-self-help-guides/sleep-problems-and-insomnia-self-help-guide if you wish further advice.
Pacing and modifying activity: This is about keeping your pain and symptoms under control. You may have ‘flare-ups’. Pacing can be achieved by following a simple traffic light system:
- Green – Pain is manageable, continue your chosen activity
- Amber – Pain is increasing, reduce your chosen activity
- Red – Pain is at high level, too much activity too soon and you need to minimise your chosen activity.
It is important not to ‘push through’ the pain.
Heat Pads: Application of gentle heat (heat pad or hot water bottle with suitable insulated protective cover) for 5 to 10 minutes on your lower back can provide muscle relaxation and pain relief. It might help to do your exercises with or after application of heat.
Avoid Smoking: Smoking increases the sensitivity of nerves which can lower your pain threshold and thus increase your pain levels. Smoking can slow down recovery and increase the release of stress hormones. Smoking can put you at risk of other adverse health conditions.
Please visit www.nhsinform.scot/healthy-living/stopping-smoking for more information or get in touch with your GP if you require assistance to stop smoking.
What treatments are available?
This type of pain generally improves over time. In the early stages, there is no specific treatment, which has been shown to benefit this type of pain apart from the advice given above. If there is no improvement after 4 to 6 weeks, you should seek the advice of a healthcare professional. If your pain does not settle, you may be referred for further assessment and treatment as appropriate. In 9 out of 10 cases, pain resolves without specialist treatment, but it can take several months to settle.
If your symptoms remain unacceptable, despite trying the advice enclosed, then further investigations and possibly surgery may be considered. This will need to consider the risks and benefits of surgery, including your general health and fitness. Surgery is most likely to benefit nerve pain in the arm, however, it is not particularly helpful for neck pain. Spinal decompression involves removal of the bone or tissue that is compressing the nerves to give the nerves more room.
How can physiotherapy help?
Your physiotherapist will provide a specific exercise programme which will assist you through the different stages of recovery. Your initial exercises will be aimed at reducing your symptoms, improving your body awareness and preparing your muscles for greater activity. As you improve tailored exercises may help to improve the mobility and strength of your neck and upper limbs.
It is important to note that these exercises should not aggravate your symptoms. You are advised to stop the exercises and contact your physiotherapist if you are not able to tolerate the exercises suggested. Your physiotherapist will be able to advise you on alternative techniques or other activities.
It is important that you play an active role in the care of your condition to aid recovery.
Following the exercises are just suggestions that some patients have found helpful in the past. Unfortunately, there are no exercises that suit everyone.
If you can tolerate alternative exercise you may prefer to undertake more general fitness type activities or exercise e.g. Pilates, Tai Chi, light gym exercises or simply graduated walking.
If you follow the exercises below and experience an increase in your symptoms, please reduce the range of movement and the number of repetitions or sets. Gradually increase these as your symptoms allow. You may need to leave it for 24 to 48 hours before trying again.
Resting Positions
Aims:
- To reduce your pain and symptoms
Ensure you have a good neck and arm position that minimises the arm discomfort as much as possible. These are usually positions that minimise or reduce the ‘stretch’ or ‘pull’ on the arm nerves.

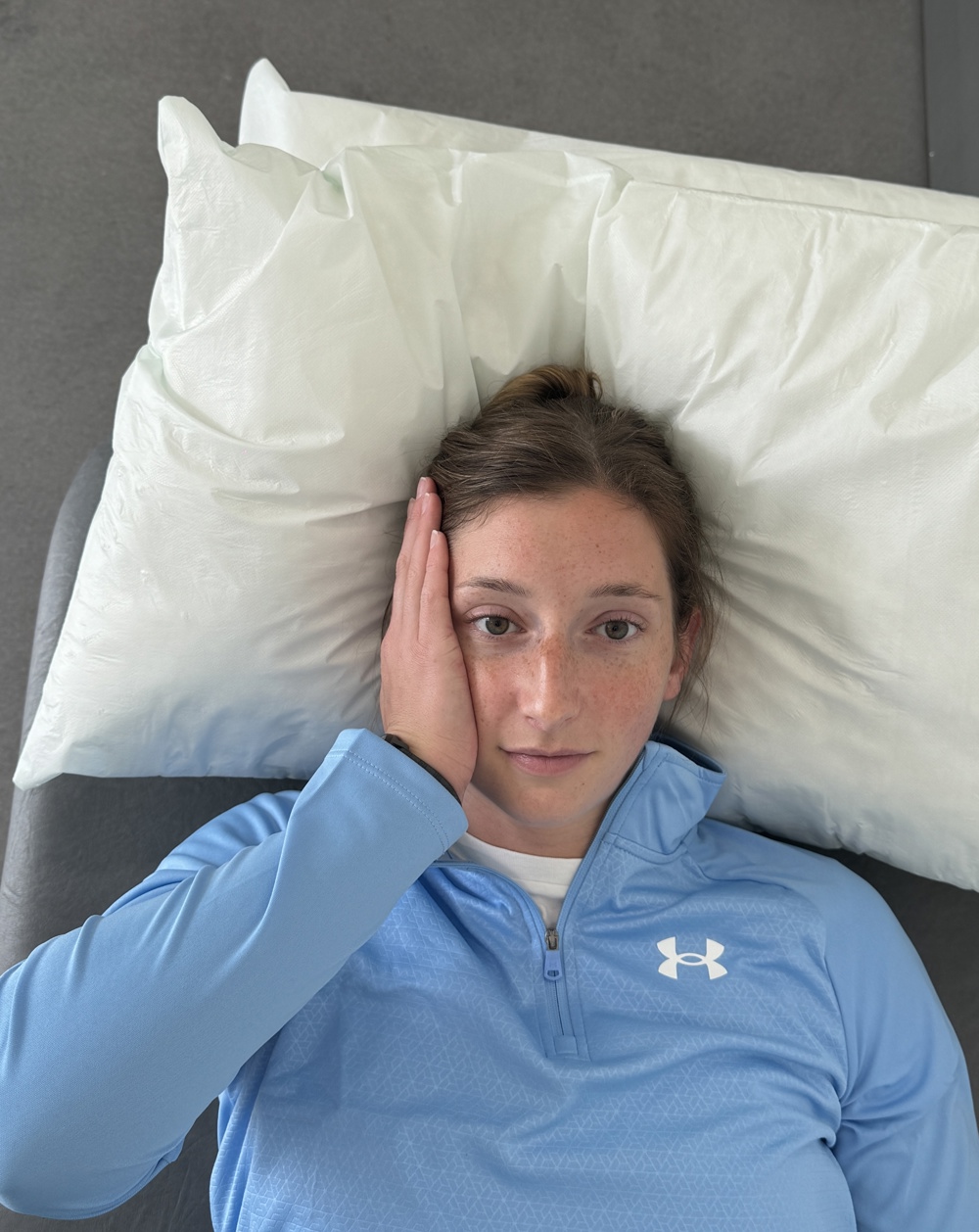
It is not uncommon to experience heaviness of your arm at rest, supporting your affecting arm on a pillow can ease that sensation.


If you prefer side lying, lie on your unaffected side or back with your affected arm resting on pillows.
Adjust the height and the position of the pillows to get adequate comfort. Some people may only need one pillow instead of two pillows.

If sitting is uncomfortable a hard straight backed chair with or without a cushion or pillow at you back may be better than a soft, low armchair. It is useful to support the affected arm by placing a pillow across your lap.
Try not to keep your spine straight and rigid at all times. This can increase muscle tension and cause further stiffening of spine.
It is important you avoid staying in one position for any length of time
Rehabilitation exercises
Aims:
- Maintain and gradually restore range of neck movements
- Maintain and gradually restore muscle activity
How often should I do these exercises?
Stretching
Start with one or two stretches held for 10 seconds and gradually build this up to a maximum of one or two sets of 30 seconds. Stretching can feel uncomfortable, but should not feel painful during or after the exercise.
Rehabilitation exercises
Try to do these exercises once a day on the majority of days. It is important to have rest days, especially if you are not used to exercising regularly. It is acceptable to break the exercises into groups and complete these at different times in the day.
Start with one set of 5 to 10 repetitions. As the exercises become easier you can either gradually increase the repetitions or add another set of exercises. A total of 45 repetitions would be a maximal effort i.e. 3 sets of 15 repetitions. Take a rest of 30 to 60 seconds between each set. Ideally the muscle(s) you are exercising should begin to feel fatigued by the end of the exercise however you should not be straining. It is normal to have some discomfort during exercises as long as it’s acceptable to you.
As you increase the repetition of exercises you should try to have a rest day after each exercise day to allow your muscles to recover.

1. Isometric neck extension
Lie on your back with your neck fully supported, with one or two pillows, and the neck slightly tipped forward (flexed) and a pillow under your knees. You may need to support the painful arm also with a pillow.
Gently push the middle of the back of your head against the bed/floor. You should feel slight tension in your neck muscles. Your head position should not move. Do not let the chin tip back.
Hold approximately 5 to 10 seconds.

2. Resisted neck flexion
Lie on your back with your neck fully supported, with one or two pillows, and the neck slightly tipped forward (flexed) and a pillow under your knees. You may need to support the painful arm also with a pillow.
Place both hands on your chin. Try to nod your head while resisting the movement with your hands. Your head position should not move.
Hold approximately 5 to 10 seconds.
3. Resisted neck rotation
Lie on your back with your neck fully supported, with one or two pillows, and the neck slightly tipped forward (flexed) and a pillow under your knees. You may need to support the painful arm also with a pillow.
Place your hand on side of your head. Try to turn your head to the side as you are resisting this movement with your hand. Your head position should not move.
Hold approximately 5 to 10 seconds.
Repeat the same steps on the other side.

4. Neck rotation
Sitting.
Turn your head to one side until you feel a stretch.
Hold approximately 5 to 10 seconds.
Repeat to other side.

5. Neck side bends
Sitting.
Tilt your head toward one shoulder until you feel the stretch on the opposite side.
Hold approximately 5 to 10 seconds.
Repeat to other side.

6. Scapula exercises
In sitting.
Move your shoulder blades gently back and down (small movement).
Hold approximately 5 to 10 seconds.
Rehabilitation Exercise Progression
Criteria for progression:
- Improving neck and arm pain.
- No worsening of arm symptoms with previous exercises.
Aims:
- Improve range of movement.
- Improve strength.
- Restore function

1. Thoracic rotation
Sit on a chair and clasp your arms on your chest.
Turn your body to the side. Follow the movement with your head and neck.
Hold approximately 5 to 10 seconds.
Repeat to the other side.

2. Shoulder abduction
In sitting or standing
Lift your arm up sideways with thumb leading the way.

3. Shoulder shrugs
In sitting or standing
Lift your shoulders and hold for 1 to 2 seconds. Then relax the shoulders again.

4. Wall press ups
Stand facing a wall with your arms straight and hands on the wall.
Do push-ups against the wall keeping your body in a straight line.

5. Thoracic (Mid) Spine Mobilisation
Crawling position.
Hollow your back. Keep your neck long and elbows straight.

6. Upper limb strengthening
Sit or stand holding your hands on your chest with ½ to 1 kg weights in your hands.
Alternating arms lift the weights from your chest straight up and bring back down.
Note: If any of these activities or exercises increase your neck or arm pain or symptoms, please stop the activity or exercise until you have discussed them with our healthcare professional.
Getting back to normal
Returning to activities of daily living
There are no specific time frames for returning to your usual activities and these vary from person to person. Symptoms may be ongoing for several months and you may need to adjust your activities and pace yourself during your recovery. Aim to increase your levels of activity gradually, avoiding worsening of your symptoms. Progress your activities as your symptoms and movements improve.
It is advisable to take regular breaks if sitting or driving for long periods of times. You may also want to take regular breaks, if you are holding your affected arm, at or above shoulder height.
Guidance for returning to work
Research suggests that staying active and keeping moving as pain allows, will help you get better sooner. Getting back to work helps most people with back pain. If you are ‘signed-off’ work, time frames for returning to work will depend on the type of work you do and a healthcare professional can advise on this. It is advised you communicate regularly with your employer to facilitate a safe and timely return to work.
Useful information
NHS Inform
www.nhsinform.scot/illnesses-and-conditions/muscle-bone-and-joints
The Chartered Society of Physiotherapy
www.csp.org.uk/conditions/managing-your-bone-joint-or-muscle-pain
Worries or concerns
Should you have any worries or concerns, please contact your Physiotherapist or GP during working hours or contact NHS24 on 111 out of working hours.
If you continue to experience problems then you should consult a healthcare professional.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
