OAB is a condition that causes you to pass urine more often than normal. There are three common problems experienced by people with Overactive Bladder.
Urgency
This is when you need to go to the toilet suddenly and if you do not get there quickly enough, the bladder muscle starts to squeeze, and you may leak urine.
Frequency
This is when you need to go to the toilet a lot but might only pass small amounts of urine. It is normal to go to the toilet between 5 and 8 times a day and once during the night (if you are under 65 years old). A healthy adult bladder should regularly be able to hold 300-600ml through the day.
Nocturia
This is when you wake up frequently overnight to pass urine.
What causes overactive bladder?
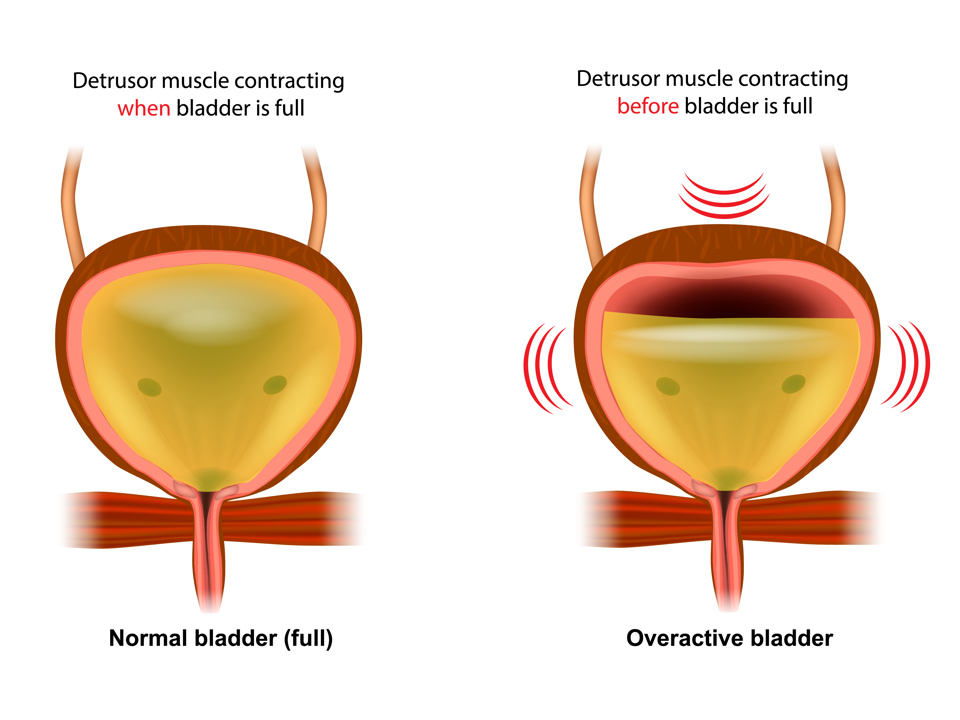
The bladder is a storage facility for urine that is produced by the kidneys. When the bladder gets to a certain capacity the bladder muscle will squeeze to send information to the brain telling you to think about going to the toilet. It is normal to be able to ignore these squeezes until it is convenient to go to the toilet. We are able to do this because the brain sends a relaxation message to the bladder telling it to STOP squeezing. With overactive bladder, the brain stops sending the relaxation message and therefore nothing tells the bladder to stop squeezing. As the squeezes are allowed to build strength and speed – your urgency will get stronger, making you feel like you need to rush to the toilet, or eventually leak.
Poor bladder habits
If you get into the habit of emptying your bladder “just in case”, the bladder gets used to holding only a small amount of urine and makes you feel like you need to go more often even though it is not full.
Certain drinks can irritate the bladder lining, making it squeeze more often, such as:
- Caffeine (tea, coffee, green tea, hot chocolate)
- Bubbles (fizzy drinks, sparkling water)
- Caffeinated energy drinks
- Alcohol
- Drinks containing sweeteners
- Fresh Acidic fruit juices (Orange Juice)

Image used with permission from bladderandbowel.org
Certain foods
Usually foods containing lots of spice, citrus, tomato, chocolate, and artificial sweeteners.
Anxiety/Stress
This is due to your fight or flight response and makes the bladder squeeze more often and with more force, causing a sudden need to go to the toilet.
Not drinking enough
This makes your urine strong and acidic which irritates the lining of your bladder even more.
Constipation, being overweight and certain medicines can significantly affect bladder function.
What can I do about it?
- Drink 1.5 to 2 litres of non-irritating fluid each day (6 to 8 mugs).
- Space your fluid intake throughout the day.
- Reduce your intake of caffeine (do this gradually to prevent headaches), aim for a maximum of 1-2 caffeinated drinks per day.
- If you wake frequently overnight to empty your bladder, try to reduce fluids 2 hours before going to bed.
- Reduce or avoid bladder irritants as listed above.
- Try to avoid constipation. Aim for 5 portions of fruit and vegetables per day and add good sources of fibre to your diet. See the NHS Fife Constipation Leaflet for further information.
- Stop smoking.
Bladder Diary
You can fill in a bladder diary to record information on your drinking and bladder habits. This will help you understand how often you are going to the toilet and how much urine you are passing. You can then practice some bladder drills to reduce your urgency and increase the time between toilet visits.
Helpful tips for holding on (bladder drills):
- Sit on a firm surface, like a hard chair, or step.
- Squeeze your pelvic floor muscles.
- Cross your legs.
- Lift your heels up and down when sitting or standing.
- Clench your toes.
- Distract yourself by thinking of something else such as counting backwards or singing a song.
- Take some deep breaths to relax your body.
Work on a bladder re-training program
Now that you have completed the bladder diary, you can see the time between your toilet visits. Most people can go 2-4 hours between emptying the bladder. Therefore, if you are going more frequently than this, you need to very slowly stretch the time between toilet visits. In order to do this, try the steps below:
- Stop what you are doing and take some deep breaths into the tummy. This helps to reduce the fight or flight response which increases the bladder spasm.
- Use some of the bladder drills above to help reduce the urge and distract you from thinking about the bladder.
- Once the urge has settled, calmly walk to the bathroom. Repeat this every time you go to the bathroom.
- Once you have mastered the calm walk to the bathroom without leakage, then you can start to put off emptying the bladder for 1-2 minutes. As this becomes easy you can gradually increase the time over a number of weeks/months.
Even putting off the need to go to toilet for 5 minutes will help to retrain the bladder. You will need to repeat this many times before it starts to become the new habit.
Be patient! It is the repeated effect of following all the advice in this leaflet that makes a lasting difference.
What else can be done?
If you have not been to your GP yet about your symptoms, it is helpful for them to see you as they may want to do some tests or rule out any other conditions that my affect your bladder. In some cases, the GP may decide that medication or skin care products may be helpful.
For people with a diagnosis of overactive bladder, up to 80% will get better by following the physiotherapy advice in this leaflet. It often takes 3-6 months to feel the most benefit.
If you are struggling to follow any of the advice or your symptoms are getting worse, then your GP may refer you to another healthcare professional for further assessment or treatment. This could include a specialist physiotherapist, nurse or doctor.
Toilet card

This card states that the card holder has a medical condition and needs to use a toilet quickly. It can help to gain access to toilets when shopping or socialising. To apply go to www.bladderandbowel.org or Tel 01926 357220.
Further information
www.nhs.uk/conditions/urinary-incontinence
References
NICE Guidance Managing OAB in Women
BAUS Leaflet 16/173 Comparison of treatment options for OAB Apr 17
BAUS Leaflet 16/002 Bladder Training Jun 17
Palma, I-A, Staack (2016) Impact of Caffeine on OAB Symptoms. Current Bladder Dysfunction Reports 11:1-7
Overactive Bladder - University Hospitals Sussex NHS Foundation Trust (uhsussex.nhs.uk)
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.

