Fife Musculoskeletal Physiotherapy
This information has been developed to supplement the information the Doctor or Healthcare Practitioner has already given you.
Issue No: 4.2.3.5.14.1
Date of Issue: February 2025
Review Date: February 2026
If the review date has passed, the content will apply until the next version is published.
Introduction
A posterolateral corner ligament reconstruction is an operation is to reinforce and stablise damaged ligaments at the outside (posterolateral) corner of the knee. Damage to these ligaments can cause pain and the knee to ‘give way’ (Figure 1).
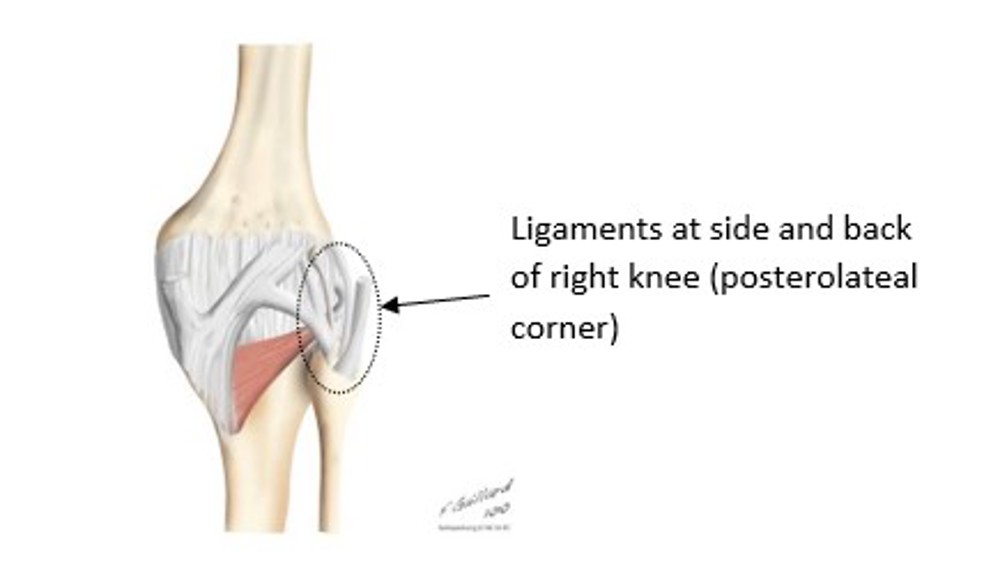
Figure 1: Diagram of back of right knee
What is a posterolateral ligament reconstruction?
The procedure usually involves using a graft for the reconstruction of the damaged ligaments. The graft can be taken either from the patient’s own body (autograft) or from a donor (allograft). Your Consultant will have discussed and agreed this prior to your operation. The autograft commonly used for PLC reconstruction is obtained from the hamstring tendon of either the leg undergoing the surgery or from the other leg. A small incision is made over the inner aspect of the knee to harvest the graft (hamstring tendon). The graft is then placed through the head of the fibula (the smaller bone of the leg) and secured to the outer aspect of the thigh bone (femur) with the help of instrumentation (screws). The wounds are then closed with sutures and dressed.
Depending on the severity of the injury a PLC reconstruction can be combined with an anterior cruciate ligament (ACL) or a posterior cruciate ligament (PCL) reconstruction, which are ligaments inside the knee itself.
Post operative advice
Following your operation, it is important for you to remain non weight bearing for the first 6 weeks to allow your knee to heal or as instructed by your Consultant Orthopaedic Surgeon. Please use the elbow crutches you have been provided with to walk.
Rest and elevation
In the first few weeks it is important to rest and elevate your leg on a stool when you are not walking or doing your exercises.
Ice packs
Ice packs can: 1) help relieve the pain and 2) reduce the swelling at your knee. To make your own ice pack wrap crushed ice cubes or a packet of frozen peas in a plastic bag and a tea towel. Apply the ice pack on your knee for 10 to 15 minutes every 2 hours.
Things to look out for when you are home
- When the dressings are removed and as the swelling goes down in the leg the brace may need to be tightened up or moved higher up your leg.
- Your wound is likely to be tender for 2 weeks. Look out for signs of inflammation, redness or leaking. If concerned contact your General Practitioner or visit your local A&E department.
- A certain amount of pain and swelling should be expected. If you notice numbness, pins and needles or lack of movement in your foot visit your local A& E department immediately.
Specific instructions
There are specific instructions the Consultant Orthopaedic Surgeon wants you to follow after your operation. These will help your recovery and allow the repaired area at the knee to heal:
- On the day of your operation, once you have recovered from the operation the physiotherapist will fit a hinged knee brace which you will wear for 6 weeks.
- The hinged brace should remain on at all times, including washing the leg and performing your exercises.
- In the shower you can wear a LIMBO cover over the brace. (limboproducts.co.uk).
- The physiotherapist will set the hinges on the brace.
Knee brace
The hinged brace (Figure 1) will be set to restrict the bend at your knee. Do not adjust it yourself.

Figure 2: Hinged knee brace
From Day 0 to 6 weeks the brace is usually set 0 to 90 degrees, but will depend on the exact surgery performed, so your Consultant Orthopaedic Surgeon may specify a different range initially.
After 6 weeks the brace will be removed by the physiotherapist or your Consultant Orthopaedic Surgeon.
Elbow crutches
The physiotherapist will teach you to use crutches. Crutches will allow you to move around following your operation.
You will be non weight bearing for 6 weeks. You must not put any weight through the operated leg.
You will be taught to go up and down stairs with crutches if this is required at home.
After 6 weeks you will gradually increase the weight through the operated leg until you no longer need the crutches. This can be approximately 10 weeks after your operation.
Outpatient physiotherapy appointment
This will be arranged about one week after your operation at a hospital near your home. It is important for you to attend these appointments as the physiotherapist will monitor your progress and give you further advice and exercises.
Orthopaedic outpatient clinic appointment
You will attend the outpatient clinic 6 weeks after your surgery where you will be seen by your Consultant. This will be sent to you by post.
Home exercises
The following home exercises should be done after your operation. Sit in a well supported and comfortable position on your bed or floor.

1. Ankle pumps
Pump your feet by pulling your toes and ankles up and down 20 times. Repeat every hour.

2. Range of motion
Bend and straighten your knee a little and often through the day as pain allows.

3. Isometric gluteal exercises
Lying on your back, tighten your buttock muscles.
Hold for 10 seconds.
Repeat 10 times.
Repeat every hour.

4. Patella mobilisations
Sitting with the thigh muscles of your affected leg relaxed move your knee cap from side to side 5 to 10 times. Repeat every hour.

5. Isometric quadriceps
Without lifting your leg off the bed, tighten your thigh muscles (quadriceps) as if trying to push the back of your knee into the bed. Avoid lifting your leg straight off the bed at this stage.
Repeat 10 times every hour.
If you are able to do Exercise 5 comfortably, progress to No: 6.

6. Straight leg raises
Tighten your thigh muscles as in Exercise 5.
Keeping your leg straight, lift the leg approximately 6 to 10cms off the bed.
Hold for 6 seconds.
Return the leg to the bed slowly.
Repeat 10 times.
Repeat exercise every hour.
Useful information
Worries or concerns
For non-urgent issues or concerns
For non-urgent issues or concerns please contact your Consultant’s Secretary through the NHS Fife Hospital Switchboard 01592 643355.
For urgent issues or concerns
If you have any urgent concerns regarding your condition, please contact the Service:
Urgent advice for patients between 8am to 8pm Monday to Sunday, contact the National Treatment Centre - Fife Orthopaedics on 01592 643355 Extension 22685.
Urgent out of the hours advice
For an urgent problem out of hours, please contact NHS 24 on 111 or attend Accident and Emergency.
Emergency advice
For emergency advice, attend Accident and Emergency or call 999.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
