Introduction
The aim of this information sheet is to give you some understanding of your shoulder problem. It will describe how to care for your shoulder after a shoulder injection (subacromial injection).
The shoulder joint comprises a ball and socket joint. Between the top of the shoulder ball and below the structures at the outer edge of the collar bone (acromion), there is a space called the subacromial space (Figure 1).
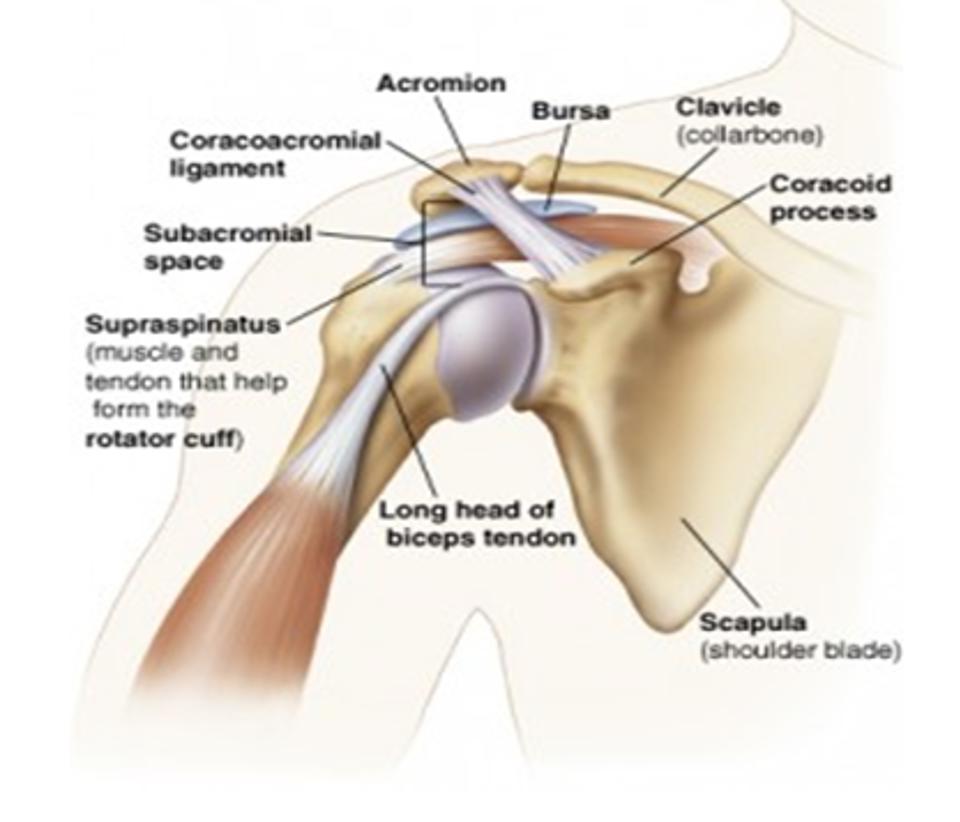
Figure 1: Shoulder and the Subacromial Space
In the subacromial space is a group of tendons called the rotator cuff tendons, which are involved in movements of the shoulder. Also, in the subacromial space just above the tendons is a fluid filled sac called a bursa. The bursa is like a thin fluid filled balloon that allows for the smooth gliding of the tendons as they pass beneath the arch during overhead movements of the shoulder.
What are the symptoms?
Subacromial shoulder symptoms vary from person to person. Commonly these include:
- Pain on moving your shoulder, especially above head height
- Pain at night, especially when lying on the affected side
- Loss of function or weakness around the shoulder, especially when lifting or twisting the shoulder or arm
What are the causes?
The shoulder is one of the most complex joints in the body and depends almost entirely on the rotator cuff (small) muscles around the shoulder to maintain stability. The most common problem of the shoulder is subacromial pain.
Normally, there is plenty of room in the subacromial space, meaning when lifting the arm above shoulder level the tendons do not rub. The space, however, can be decreased by age related changes and or irritation and swelling of the tendons and/or bursa between the shoulder and the acromion bone.
There can be many reasons that you develop subacromial pain, including trauma, age related changes and/or overuse. Sometimes there is no obvious cause. 20% of people will develop these symptoms at some time in their life.
What does the injection procedure involve?
The Orthopaedic team will have discussed that a subacromial corticosteroid (steroid) injection is a beneficial treatment option and explained the procedure to you. Two different types of medication are usually injected into the subacromial space of the shoulder. The medications consist of a steroid (e.g. Depomedrone, Kenalog) and a local anaesthetic (e.g. Lidocaine, Levobupivacaine) (Figure 2).
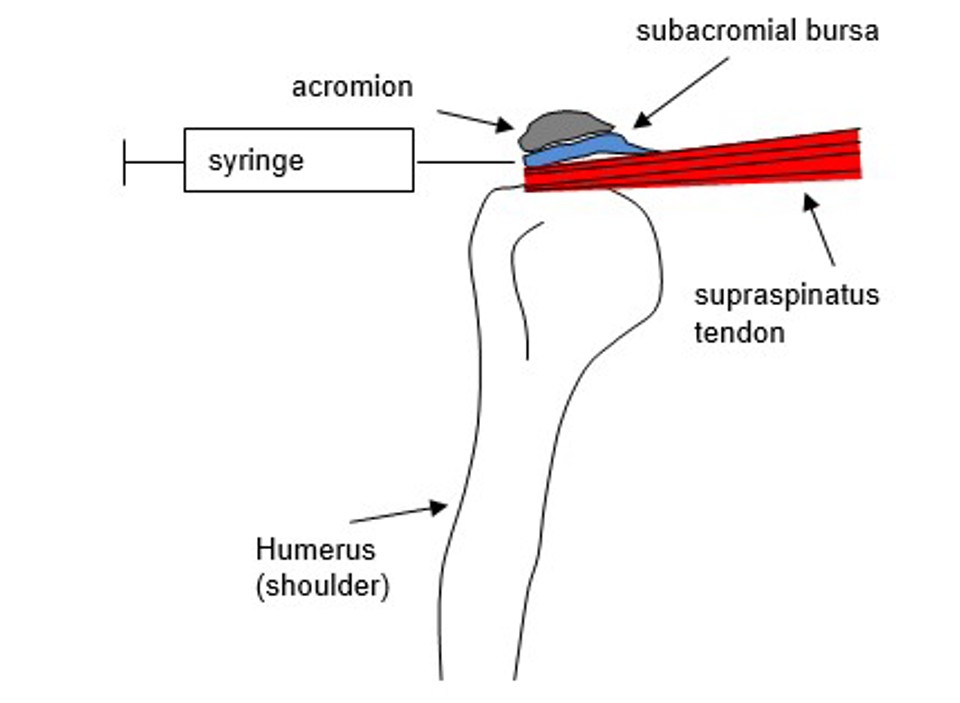
Figure 2: Front View of the Shoulder and Syringe Injection into Subacromial Space
Why am I having an injection?
The purpose of the injection is to provide you with pain relief. The steroid works as a powerful anti-inflammatory to reduce any swelling in the shoulder, and the local anaesthetic helps to spread the steroid around the shoulder and will potentially provide short term pain relief. The injection can also help you to engage with some strengthening and movement exercises, which will help your pain in the longer term.
Are there any risks associated with having the injection?
As with all treatments, there are risks associated with the procedure, however, subacromial steroid injections are recognised as low-risk procedures.
The main risks associated with subacromial injections include:
- Allergy to the medication
- Infection (e.g. new onset of increased heat, swelling or redness at shoulder joint)
- Tendon weakening / rupture
- Raised blood sugars in diabetic patients
- Menstrual irregularities
- Syncope (fainting)
What should I do or expect after injection?
The steroid usually starts working within 24 to 36 hours after the injection and continues to have an active impact for 3 to 4 weeks.
The benefit is variable, some people will get short term relief, for other people, the injection will alleviate the pain completely.
The local anaesthetic may numb the pain in your shoulder temporarily. We recommend that you do not do anything with your shoulder immediately following your injection that you could not do before your injection.
We recommend you wait until 2 weeks after your injection before gradually returning to your sport or full activities. The injection can temporarily weaken your tendons therefore wait 2 weeks after your injection to return to moderate activities and 3 to 4 weeks to return to any sporting activity e.g. racket sports, gymnasium weights.
The general exercises outlined below are recommended for people following subacromial injections.
You may be referred for physiotherapy following your injection. Your physiotherapist will advise you as to whether to continue with the exercises outlined below or not.
Exercise advice after injection


Exercise 1 - Wall slides
Find a smooth wall or wall mirror and a cloth that will slide easily on the wall (or put clean socks on your hands). Stand facing the wall. Place the edges of your hands against the wall with your thumbs facing you.
Now step forward as you gently push into the wall and slide your hands up as far as you can. Relax and return to the starting position
- Repeat 8 times
- Rest for a minute
- Repeat 8 times
- Rest for a minute
- Repeat 8 times
When you can do this exercise easily you can progress by doing it without the support of the wall and adding a light weight.


Exercise 2 - Shoulder push ups
Now put your hands on the wall as if you are going to do a push up. Make sure your hands are placed a little wider than the width of your shoulders, your hands are turned out slightly and your elbows are below your shoulders.
Now lower your body towards the wall keeping your body nice and tall.
- Repeat 8 times
- Rest for a minute
- Repeat 8 times
- Rest for a minute
- Repeat 8 times
When you can do this exercise easily you can progress and increase load by moving your feet further from the wall.


Exercise 3 - Shoulder rotations
Sit next to a table with your elbow supported just below shoulder height on a rolled up towel.
Now make a gentle fist, keep your elbow bent and then rotate your forearm to point upwards.
Return to the start position and relax.
Make sure you sit up tall whilst you do this.
When it is easy for you to do this you can add a light weight – start with a half kilogram weight or a small 500ml water bottle.
As the exercise gets easier you can increase the weight:
· First to 1 kilogram
· Then to 1 and half kilograms
· Then to 2 kilograms.
The key to success and getting the most from your injection and exercises
- Build the exercises into your daily routine so you can do them regularly.
- Find time when you are not under pressure and can give the exercises your full attention.
- Try to do the exercises on six days each week with one day off. If you want to get better, you will need to do them on at least four days of the week.
- You do not have to do all three exercises straight away – you can start with two and build in the third when you get confident.
- It helps to keep an exercise diary to record how many repetitions you have done and see how you are progressing.
- If one particular movement causes more pain, then use it each week to test if you are improving and getting better.
Worries or Concerns
For Non-Urgent Issues/Concerns
For non-urgent issues or concerns please contact your Consultant’s Secretary or Healthcare Practitioner through the NHS Fife Hospital Switchboard 01592 643355.
For Urgent Concerns
If you have any urgent concerns regarding your injection, please contact the Service:
Urgent advice for patients with injection problems between the hours of 8am to 4pm Monday to Friday please contact the National Treatment Centre-Fife Orthopaedics 01592 643355 Extension 22685.
Urgent advice for patients with post injection problems between the hours of 4pm to 8pm Monday to Friday, Saturday, Sunday and Public Holidays 8am to 8pm please contact National Treatment Centre-Fife Orthopaedics - Advanced Nurse Practitioner 01592 643355 Extension 22685.
Urgent Out of the Above Hours Advice:
For an urgent problem out of hours please contact NHS 24 on 111 or attend the Accident & Emergency Department.
Exercises adapted from ‘BESS Exercises for Shoulder Pain by Rees, J., Kulkarni, R., Gibson, J. and Connor, C. Supported by Barker, M. and Yates, R. (2018) Permission granted with thanks Sept 2023.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
