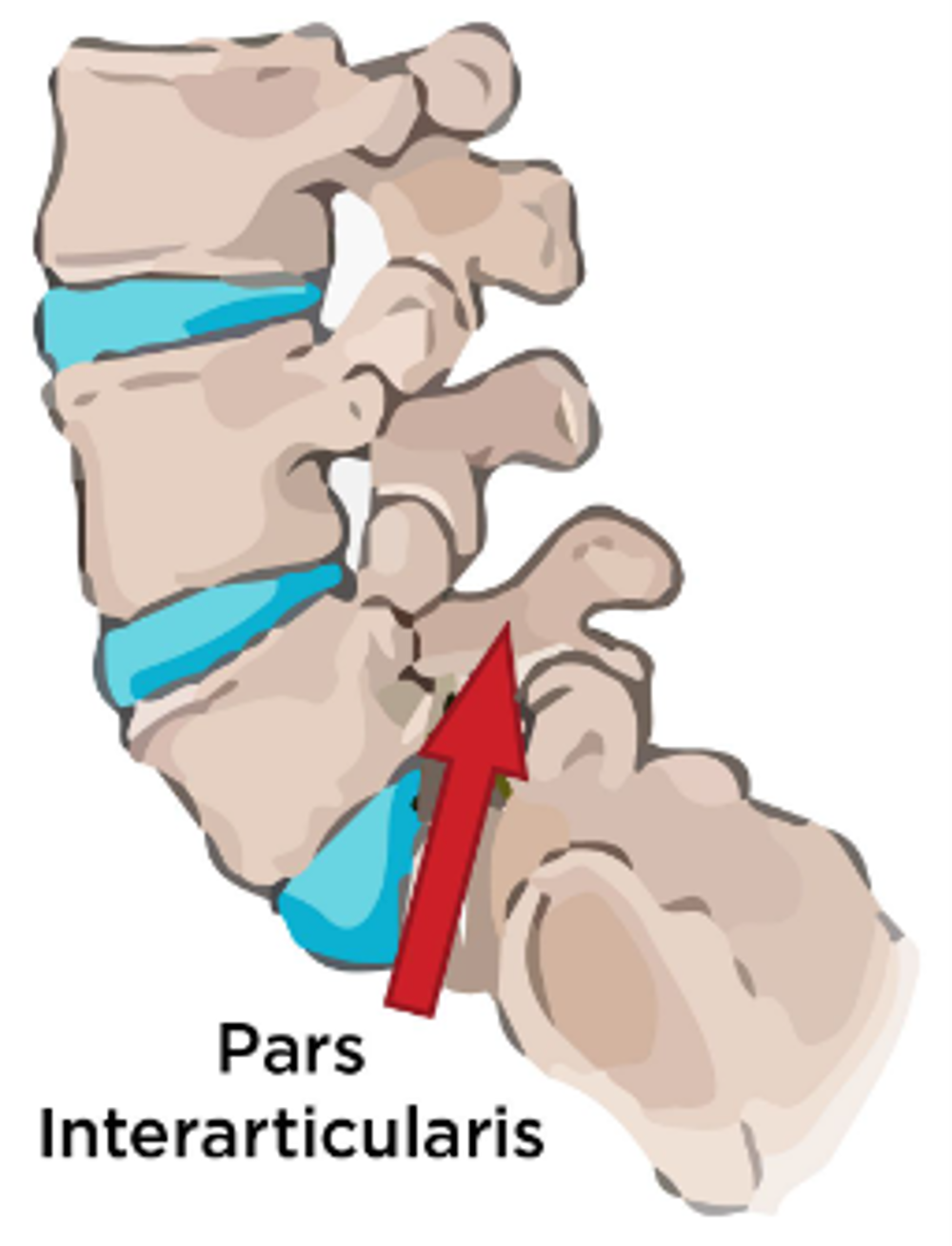
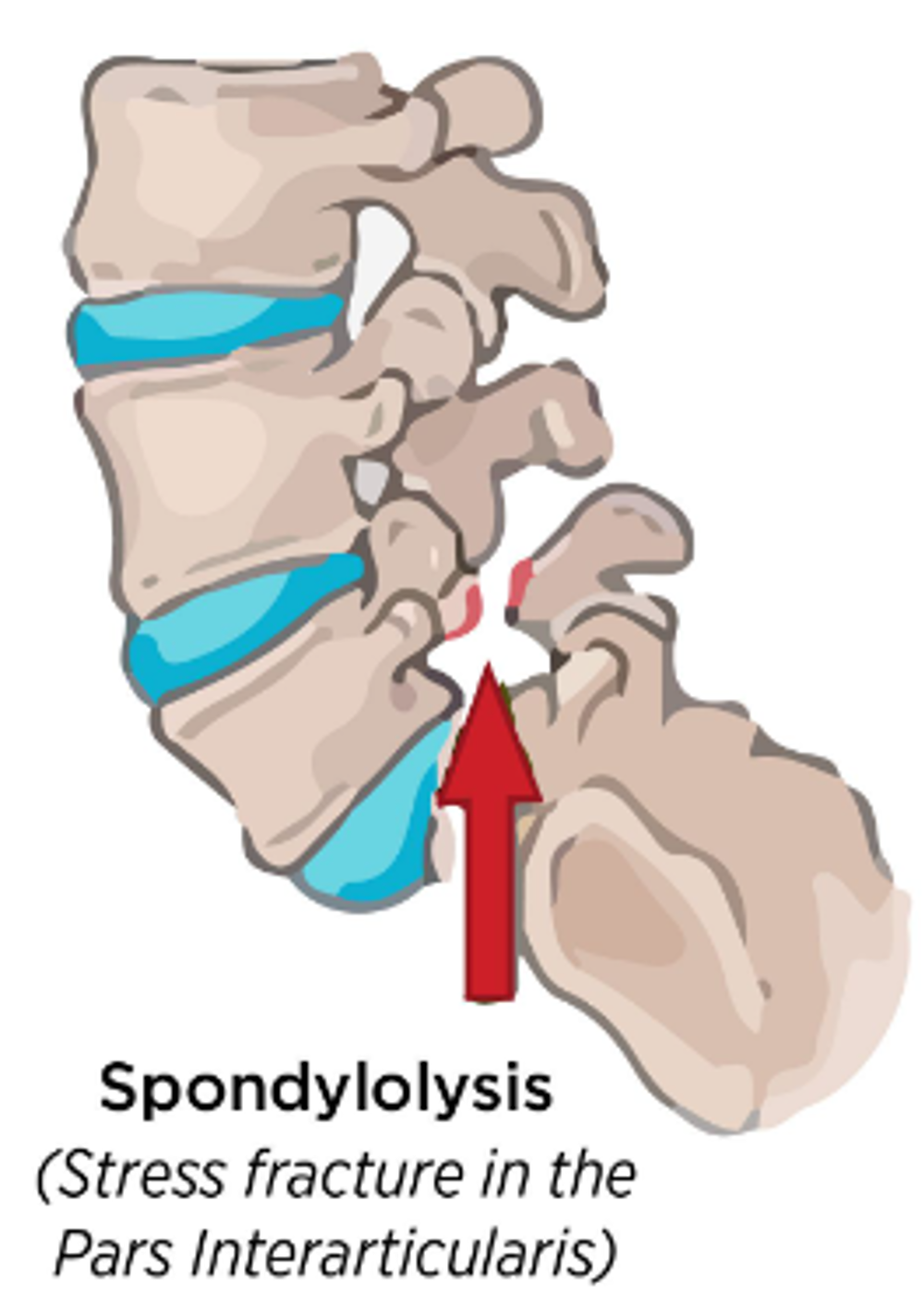
What is a Spondylolysis/Pars Defect?
A pars defect or spondylolysis is a stress fracture of a specific area of the bones of the lower spine. They can be on one or both sides of the vertebrae.
While it is a recognised cause of low back pain in children and adolescents, by far the most common cause of low back pain is simple muscle pain.
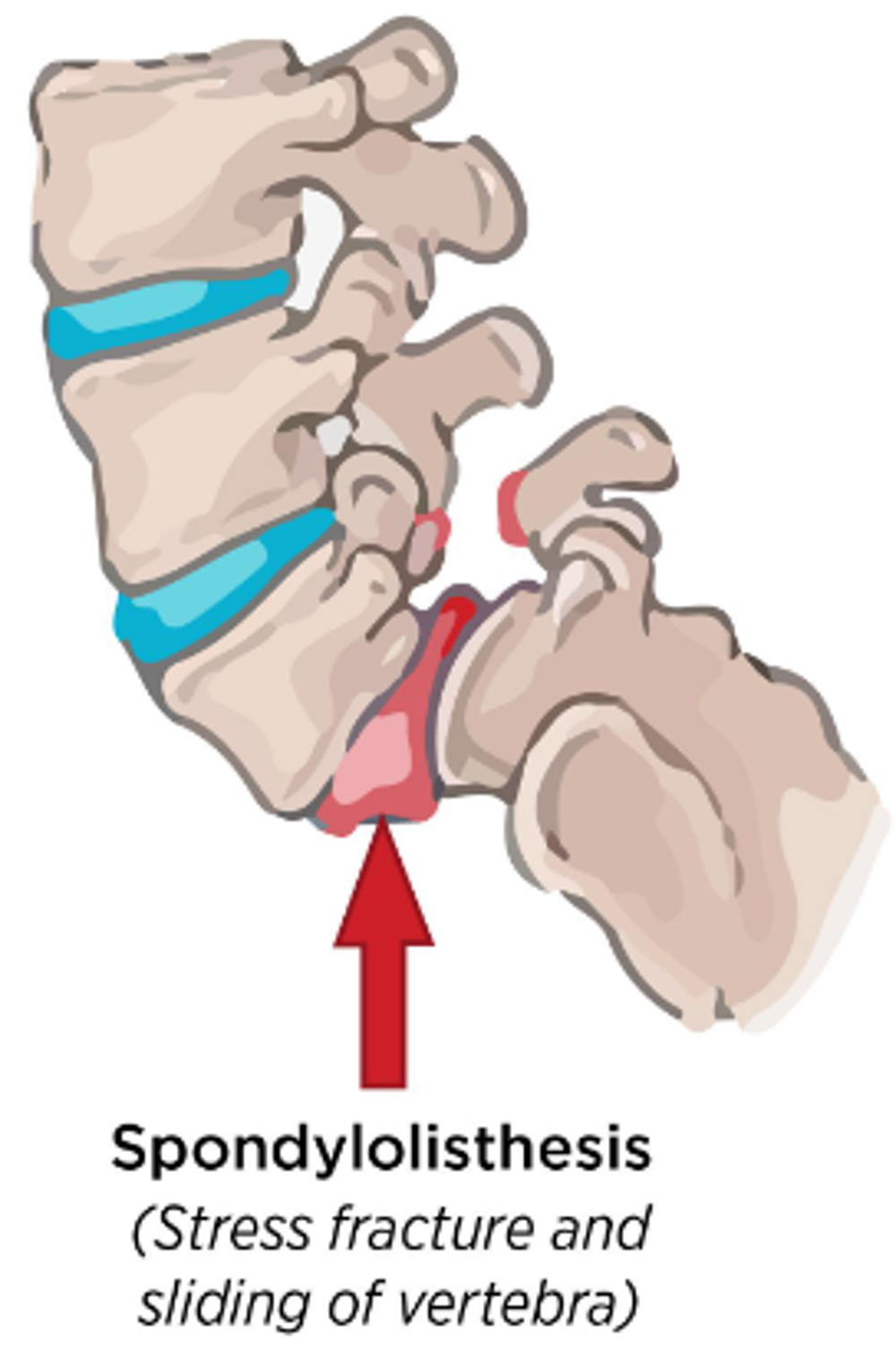
What is a Spondylolisthesis?
Spondylolisthesis is where one of the bones in your spine, called a vertebra, slips forward. This is very rare and occurs only in the presence of a spondyloysis on both sides of the vertebrae.
What is the cause?
We don’t know for sure but there is thought to be a link between certain activities and overuse of the lower back. Stress fractures are tiny cracks in a bone caused by repetitive force or overuse. Sports that include a lot of rotation or extension of the lower back can be a cause.
What are the symptoms?
The main symptom is low back pain that worsens with activity and improves with avoiding the sport/activity that causes repeated back bending. Sometimes the pain can spread down the back or side of the thigh.
How is the diagnosis made?
The clinician may be suspicious from your symptoms and certain findings on examination might suggest this as a cause of the back pain. Pain on extending the lower back and marked tightening of the hamstrings can be signs of possible spondylolysis.
Your clinician may request an MRI scan of the lower back to confirm or exclude the diagnosis if they are sufficiently suspicious this might be the cause.
X-rays are usually not a first line investigation for spondylolysis as they are not very good at picking up the condition. If spondylolysis is confirmed on MRI, it is possible that further tests including a CT scan or specific X-ray may be requested or used for follow up as this can show further details of the condition of the healing bone.
What is the treatment?
Symptomatic management in terms of avoiding activities that make symptoms worse and keeping pain under control is the main course of treatment initially.
A referral to Physiotherapy may help you manage your symptoms and advise on rehabilitation.
They can provide exercises to strengthen and stretch the muscles in your lower back, tummy and legs during the healing period. Your physiotherapist will also discuss pacing activities and give parameters for recommended activity levels.
Any return to sport will be based on symptoms as well as the results of any imaging. This will be discussed with you at each Orthopaedic clinic.
What is the long term impact?
Almost all spondylolysis will heal over a period of a few months with a reduction of sporting activity. It may be necessary to avoid sport entirely until healing has occurred. Your clinician will be guided by your symptoms but may use investigations like CT or x-ray to monitor the progress of healing.
In a few cases, the condition can be slow to heal or allow some abnormal movement between the vertebral bones (spondylolisthesis). Time may still allow complete healing but for a very small number of patients, an operation might be discussed. This would usually only be considered if there was no sign of healing after 6-9 months or more than 25% of abnormal movement between the bones is seen.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.





