A broken hip is a common injury. It can occur after even a minor fall, if the bone is weak. Approximately 35 patients every month are admitted with a broken hip to the orthopaedic wards here in Victoria Hospital.
It is usually recommended that you have an operation for your broken hip. This will be done as soon as possible after your admission.

A nurse will be allocated to care for you
The nurse and ward doctor will ask some questions and examine you. They will explain what will happen to you and will answer any questions you may have. You will have a tracing of your heart, blood samples taken and any other tests that may be necessary will be organised.
You will be offered a painkiller. This is normally given as tablets or a liquid.
On the day of your operation the doctor will decide when you will stop eating and drinking. You may have a drip (intravenous fluids) overnight.
Some patients find it difficult to pass urine whilst in bed. If you find this a difficulty you will be catheterised (a small tube is passed into your bladder and it will take your urine away into a collecting bag).
The anaesthetist will come and see you in the morning of your operation to discuss what kind of anaesthetic you will have.
The most common types are either a:
- Spinal (numb from the waist down) with sedation (to make you sleepy)
- General anaesthetic where you will be asleep.
Your Consultant will decide and discuss with you the type of operation you will have to repair your hip (see page 2).
Your nurse will prepare you for theatre by helping you into a theatre. gown, and you will be taken to the operating theatre in your bed.
After your operation
On your return to the ward you will be made comfortable. You may need oxygen until you are fully awake.
You will have a cannula in your arm and receive fluid through a drip. Once awake you can eat and drink.
The nurse will regularly check your blood pressure, pulse and _wound dressing. Usually painkilling tablets or liquid are prescribed and given regularly, but if you are sore please tell a nurse.
The first day after your operation your rehabilitation begins.
You will meet your:
- Physiotherapist (physio) - who will help you try to regain the level of mobility you had before you broke your hip.
- Occupational Therapist (O.T.) - who will help you increase your independence in everyday tasks
Everyone recovers at a different pace therefore please don't compare yourself with others.
Your rehabilitation will take place initially in ward 31 Victoria Hospital which is the Acute Hip Fracture Ward.
Day one
You will be helped out of bed on the first day after your operation. Your drip will be removed if you do not need further fluid or a blood transfusion. Your wound will be inspected and the dressing checked as required. If you have a shower then it may need changed. You may have a catheter in your bladder. This will be removed once your bowels have moved and you are starting to walk.
In order to plan for your discharge.the Occupational Therapist will ask about your home circumstances and what you were able to do before your injury or fall. This will help. us plan your rehabilitation.
Your Occupational Therapist will ask you to arrange for your clothes and a pair of flat comfortable shoes to be brought in, as soon as possible.
Your Physiotherapist will:
- Ask you to move your toes and ankles to improve your circulation. This reduces the risk of a blood clot forming in your leg.
- Teach you how to tighten your thigh muscles.
- Help you to gently bend the knee of your affected leg.
- Encourage you to help the nurses as much as possible while moving in bed.·
- Help you to stand with the aid of a frame or stand aid and help you sit in the chair if you are feeling able.
Days two and three
You will be assisted out of bed to sit in a chair. The physio will help you to stand with a frame or stand aid and you will be encouraged to take a few steps. You will continue with bed exercises.
The Occupational Therapist will show you the easiest and safest way to wash and dress yourself. The therapists will help you practice sitting and standing. You will gradually increase the distance you can walk with the frame and you will continue with regular exercises when you are in bed and in your chair.
The Occupational Therapist will see you daily, if required, to increase your independence with self care tasks. You will be shown the best way to manage getting on and off the bed and toilet if you were independent before coming in to hospital.
Further progress
As you progress you will attend the gym to improve your walking using the parallel bars, do further exercises and balance activities. Your muscle strength will be tested and you n:,ay do some exercises with weights to improve your strength.
Slow Progress and Down Stream Beds in the Community Hospitals
Before breaking your hip you may have suffered from other illnesses, falls and a poor ability to walk. This can slow your recovery. You may benefit from moving to a community hospital, where you will have further rehabilitation, with more time to reach your potential and prepare for going home.
These Down Stream Beds are at Adamson, Cameron, St Andrews Community, Glenrothes and Queen Margaret Hospitals. A member of the Orthopaedic Hip Fracture team will make the referral for a downstream bed and keep you informed.
Getting on and off your chair
- Step back until your feel the back of your chair with your legs.
- Reach back one hand at a time and feel for the arms of your chair.
- Place your operated leg out in front of you.
- Lower yourself down slowly taking your weight through your good leg.
- To stand up remember to lean forward and push up using your hands and both legs.
Getting in and out of your bed
-
- Sit on the edge of your bed.
- Try and slide yourself into the middle of your bed using your arms and good leg.
- Keep your legs together and swing them onto your bed.
- If necessary use your hands to lift your operated leg.
- To get off your bed remember to lean forward and push yourself up using your hands and both legs.
- Sleeping -you will find it most comfortable to lie on your good side with a pillow between your knees, or on your back.
Advice on staying safe at home
The risks of falling can be reduced by making your home free of potential hazards. You can do this by:
- Lifting any loose rugs
- Tacking or using carpet tape to secure any loose carpet edges
- Tucking away any loose cables or electrical flexes
- Making sure there is adequate lighting at all times and that you can reach all switches
- Taking your time when sitting to standing and moving about and always use your walking aid which has been provided
- Use a rubber mat in the bath or shower. Wipe up spills of water straight away
- Having good handrails preferably on both sides on the stairs and take particular care when you reach the top and bottom steps
- Asking for help if you think you might not manage a task, e.g. cleaning curtains/cupboards or putting out rubbish
- Visit your optician regularly
Getting ready for discharge home
As you progress the therapy team will discuss what you need to achieve to get home, e.g. being able to get washed and dressed, how far you need to walk and if you have steps or stairs.
Depending on your progress the distance you walk will gradually be increased. If you are confident and depending on how well you walked before your broken hip you may progress to using 2 walking sticks before you go home.
If you have stairs at home then you will practice stair climbing before your discharge.
Going upstairs
- One hand on the bannister and a stick in the other
- Take one step at a time
- Step up with the good leg first
- Then the operated leg
- Finally the stick
Going downstairs
- Put the stick down first
- Then the operated leg
- Then the good leg down
Planning for discharge
The therapy team may also speak with your family or carers about your home environment and any support you may need.
The Occupational Therapist will arrange any necessary equipment that is required for home, e.g. commode, raised toilet seat, and will discuss delivery arrangements.
You will not be discharged until you and all the staff caring for you. are happy that you will be safe.
After going home further rehabilitation may be necessary
This will be organised before your discharge and the options discussed with-you.
- ICASS - The Integrated Community Assessment and Support Services This team provides a short term level of support for you in your own home when you are discharged from hospital. Depending on your needs, nurses, physiotherapists, occupational therapists, and rehabilitation assistants may be arranged for you. This is to provide further support and rehabilitation when you are at. home.
- Community Physiotherapy - this will be arranged by the physiotherapist. You will be seen at home but it may be up to two weeks before the community physiotherapy team can visit.
- Day Hospital - further rehabilitation from therapists in a
hospital setting - 1 or 2 times per week. - Out Patient Physiotherapy - at your local hospital or GP surgery
Home exercise programme
Do these exercises three times a day
Lying on your bed, using a slippery surface such as a tray, bend your operated leg up and down. Repeat five times.
Lying on your bed keep your leg straight and slide it out to the side and back. Repeat five times.
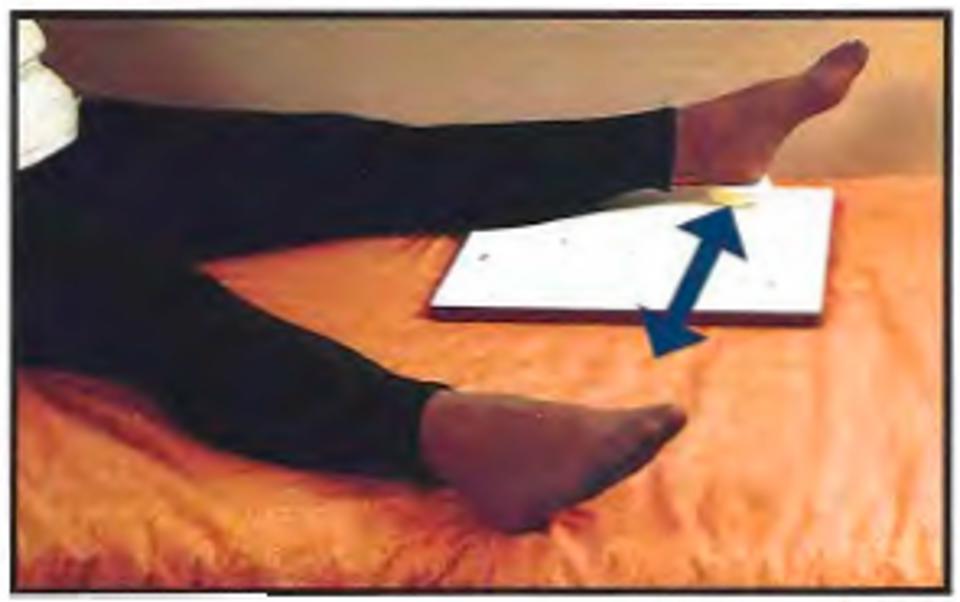
Lying on your bed, with a rolled up towel under your knee, raise your heel off the bed and straighten your operated leg. Always keep your thigh resting on the towel. Repeat 5 times.

Sitting in your chair with your knees bent, straighten the knee of your operated leg. Repeat 5 times.
Accessible formats
If you require this information in a community language or alternative format such as Braille, audio, large print, BSL, or Easy Read, please contact the Equality and Human Rights Team at: email: fife.EqualityandHumanRights@nhs.scot or phone 01592 729130. For people with a hearing or verbal impairment you can also contact the team through the NHS Fife SMS text service number on 07805800005.
